In this post, I again review and excerpt from The Cribsiders‘ #49: Appendicitis – Tips and Tricks For When It’s the Appendix, APRIL 27, 2022. By SAM MASUR.*
*Lim J, Fishman M, Kelly JM, Hirsch A, Nandivada P, Masur S, Chiu, C, Berk J. “#49: Appendicitis – Tips and Tricks For When It’s The Appendix.” The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ April 27, 2022.
All that follows is from the above resource.
Summary
Does abdominal pain give you abdominal pain?
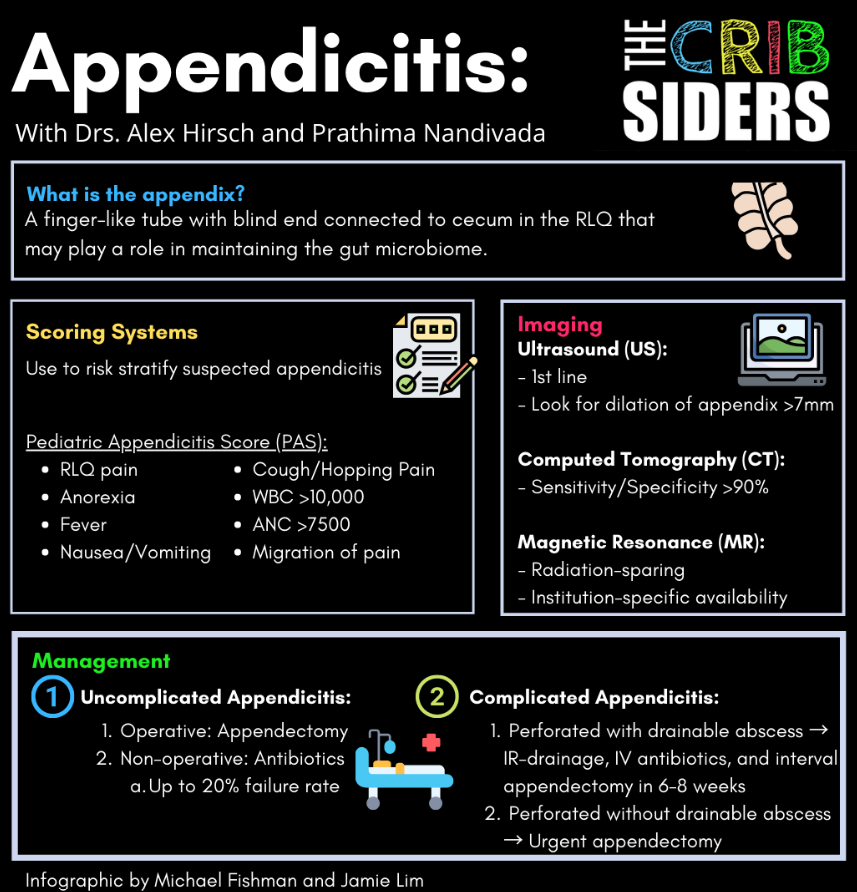
Not to worry, Dr. Alex Hirsch, pediatric emergency medicine physician, and Dr. Prathima Nandivada, pediatric surgeon extraordinaire, are here to remind us what the appendix is, what happens when it goes wrong, how to manage it, and more in this gut-wrenching episode.
Appendicitis Pearls
- While textbooks teach that right lower quadrant pain, anorexia, and pain with coughing/jumping are the classic presentation of appendicitis, presentations can also mimic gastroenteritis, constipation, and UTI, so have a low threshold to keep appendicitis on your differential for pediatric patients with abdominal pain, as appendicitis is a must-not-miss diagnosis (especially in those tricky toddlers!).
- Validated scoring systems like the Pediatric Appendicitis Score (great for bedside use) and the Pediatric Appendicitis Risk Calculator (more accurate, but cannot be done at the bedside) are important tools to help risk-stratify patients.
- In settings with experienced sonographers, ultrasound is a great first step to evaluate for signs of appendicitis or secondary signs of inflammation, but cross-sectional imaging (CT or MRI) may be needed to further confirm/evaluate.
- Appendectomy is the treatment of choice for acute uncomplicated appendicitis. Non-operative management with antibiotics may have up to a 20% failure rate and requires a reliable, well-informed family and shared decision making. Appendicolith and major appendix dilation are contraindications to non-operative management.
- There are racial disparities in the management of appendicitis. Minority children are more likely to be diagnosed with perforated appendicitis, less likely to undergo a laparoscopic procedures, and less likely to receive opioid pain medications.
Appendicitis Notes
Anatomy/Physiology
Normal Anatomy/Physiology
Finger-like tube with a blind end connected to the cecum in the right lower quadrant. It was thought to be a vestigial organ, although recent research demonstrates that it may function in maintaining the gut microbiome. Research shows that those with a history of an appendectomy may be at higher risk for Clostridioides difficile colitis (Heindl, 2020).
Pathophysiology of Appendicitis
Appendicitis is inflammation of the appendix. Importantly, it does not indicate the cause of the inflammation, which could be fecalith, tumor, lymphoid tissue, or secondary inflammation from adjacent ileitis, peritonitis, etc. Up to 8% of children presenting with abdominal pain will have appendicitis, but it is rare in infancy (Lee, 2021). The lifetime risk of appendicitis is around 7-10% (Addiss, 1990).
Diagnostics
History
Consider appendicitis in a child with abdominal pain and/or tenderness (not just nausea and vomiting). Common features in the history of present illness include: migration of pain to the right lower quadrant (RLQ), localization of pain in the RLQ (though not always), anorexia/decreased appetite, nausea/vomiting, cough/hopping pain, and fever. Expert opinion: have a low threshold to consider appendicitis, as it can be a challenging and humbling diagnosis.
Toddlers are especially challenging to diagnose appendicitis in, as history, physical exam, and IV placement can be difficult in this age group. One particular red flag to look out for in the toddler age group is the refusal to walk or difficulty walking (indicating possible peritoneal signs).
Exam
Look for passive signs of tenderness (RLQ rigidity, involuntary guarding), and pain on palpation when distracted. Point tenderness is not always in the RLQ. Abnormal gait (a child hunched over) is concerning for appendicitis. Specific exam maneuvers (e.g. psoas/obturator sign) are good to know, but not overly sensitive or specific.
Scoring Systems
Different scoring systems exist to risk-stratify patients with possible acute appendicitis:
PEDIATRIC APPENDICITIS SCORE (PAS): WELL VALIDATED, USES A COMBINATION OF HISTORY, PHYSICAL EXAM, AND LAB FINDINGS THAT CAN BE INCORPORATED AT THE BEDSIDE IN A SIMPLE POINT SCORING SYSTEM. EDITOR’S NOTE: PAS USES WBC > 10,000 AND ANC > 7,500 AS RISK FACTORS FOR APPENDICITIS (SAMUEL 2002).
PEDIATRIC APPENDICITIS RISK CALCULATOR (PARC): OUTPERFORMS THE PAS SCORE; HOWEVER, INPUTS AND RISK CALCULATIONS ARE MORE COMPLICATED, AND THUS IT REQUIRES A CALCULATOR SUCH AS MDCALC OR THE EMR (KHARBANDA 2018).
Imaging
POINT-OF-CARE ULTRASOUND (POCUS)
Many providers feel comfortable using POCUS to risk stratify suspected appendicitis and hasten workup, antibiotics, and surgical consults.
FORMAL ULTRASOUND
Look for dilation of the appendix (>10mm is likely an inflamed appendicitis, <7mm is likely not inflamed, anything in between is more of a gray area) and any secondary signs (including fat stranding, presence of appendicolith, free fluid, etc). Make sure to follow the appendix back and demonstrate it comes from the cecum, as terminal ileitis may mimic appendicitis on ultrasound.
If the ultrasound is equivocal, Dr. Hirsch treats symptoms (e.g., ibuprofen, fluids, and ondansetron) and re-assesses using time as a diagnostic tool. If pain persists on re-assessment, then further imaging is needed, which is often institution-specific.
COMPUTED TOMOGRAPHY (CT)
CT is technically the gold standard, with sensitivity and specificity >90% (Mittal 2019). CT is usually obtained after an equivocal US.
Magnetic Resonance Imaging (MRI)
Many pediatric hospitals are moving towards using MRI if ultrasound is equivocal. Some institutions consult pediatric surgery to help determine whether or not to obtain an MRI. MRI has great test characteristics and has the added benefit of sparing radiation, though is less commonly available. Editor’s note: There are many institution-specific pathways for the evaluation of suspected appendicitis.
Surgical consult
Dr. Hirsch will involve surgical colleagues earlier if the pre-test probability for acute appendicitis is high or if he has clinical concern that necessitates prompt management. In practice, a surgical consult is often deferred until after imaging and initial lab work have been completed. For equivocal cases, surgical colleagues can be helpful to guide next steps, including further imaging, work-up, or disposition (discharge with close follow-up vs admission for serial abdominal exams).
Mimics of Appendicitis
Mimics of appendicitis include viral gastroenteritis, constipation, UTI, mesenteric lymphadenitis, renal colic, and Meckel’s diverticulum. Don’t miss ovarian or testicular torsion!
Management
The first step is deciding between uncomplicated vs complicated appendicitis. Complicated appendicitis is defined as perforated appendicitis, periappendicular abscess, or peritonitis.
Antibiotics
Antibiotics should be given as soon as the diagnosis is made, regardless of the operative choice. Antibiotics should cover gram-negative and anaerobic bacteria (intra-abdominal flora) and may vary depending on institutional practices, availability, and individual patient factors such as allergies. Options may include:
- Piperacillin + Tazobactam
- Ceftriaxone + Metronidazole
- Cefoxitin
Uncomplicated Appendicitis
Operative management: For uncomplicated appendicitis, first-line treatment is laparoscopic appendectomy. The operative risk is very low, the surgery is highly successful (most kids go home from the recovery room), and long-term risks (e.g., small bowel obstruction from adhesions) are rare. Negative appendectomy rates are very low (Childers 2019).
Non-operative management: Occasionally, for families who strongly prefer non-operative management, management with antibiotics only can be considered. Dr. Nandivada does NOT offer non-operative management if there is an appendicolith or appendiceal dilation of >11mm. Around 10-20% of children treated nonoperatively have recurrent appendicitis (Podda 2019). Dr. Nandivada will treat well-appearing children with a 7-day course of amoxicillin/clavulanate. If kids are not better in a few days, Dr. Nandivada will repeat labs and imaging.
Complicated Appendicitis
There is more variability and less clarity in the management of complicated appendicitis.
Urgent Appendectomy: If the patient has perforated appendicitis without a well-defined drainable abscess (likely is an “early” perforation in a child with symptoms for ~<3 days), Dr. Nandivada still offers urgent appendectomy, as studies show that urgent appendectomy is not inferior to interval appendectomy (Blakely 2011). An urgent appendectomy may also be indicated depending on the patient’s clinical status.
Interval Appendectomy: For perforated appendicitis with a closed-off abscess with a well-defined rind (where it is likely a late perforation and the operative risk is high), initial treatment is typically percutaneous IR drainage, IV antibiotics, and then interval appendectomy in 6-8 weeks.