In this post, I review and excerpt from The Cribsiders‘ #16: Kawasaki Disease with Recrudescent Guest Dr. Tremoulet, JANUARY 6, 2021, by DR JUSTIN BERK.
All that follows is from the above resource.
Summary
With a persistent fever, Kawasaki Disease must be on your differential, but
[what if you have] not seen many cases or [have] had difficulty with the diagnosis? Look no further, as we bring an expert to walk us through the diagnosis and management of KD! We discuss Kawasaki Disease with Dr. Adriana Tremoulet who is the assistant director of the Kawasaki Disease Research Center at the University of California, San Diego. She has led numerous Phase I through III trials regarding the management of KD, and she walks us through the diagnosis and management of this fascinating disease!
Kawasaki Disease Pearls
- Take a detailed history since the signs and symptoms of Kawasaki Disease can come and go. (Be sure to check any pictures the parents may have!)
- When you are performing the physical examination, be sure to look for the criteria but also be on the look-out for signs of an alternative diagnosis.
- In a patient with incomplete Kawasaki Disease, further work-up and treatment is indicated to identify all patients who are at risk for coronary artery aneurysms.
Core Criteria of Kawasaki Disease
“The eyes cannot see what the mind does not know.”
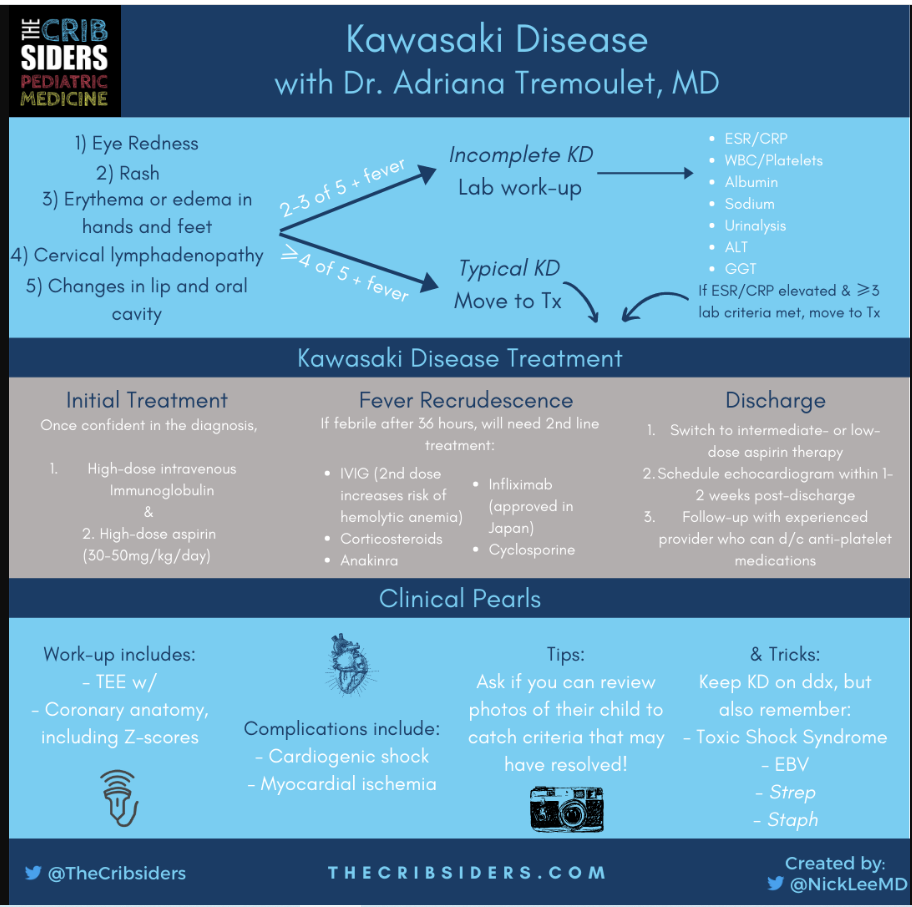
The first step to diagnosing Kawasaki Disease (KD) is to include it on the differential that we are creating. Once you’ve done that, on your history and physical evaluate for the five core criteria (in addition to fever):
Eye redness
- Typically, both eyes become red at the same time without sick contacts or discharge
- “Limbic sparing” because it is technically injection and not conjunctivitis (no inflammation of conjunctiva in KD)
- Unilateral eye redness, one eye being more red than the other, sick contacts, or eye discharge is more suggestive of a acute viral etiology and not KD
Rash
- More prominent in the genitourinary area, so it is important to look underneath the diaper
- There is no classic KD rash, although it is not vesicular.
- Less likely KD (and more likely viral infection) if there are dots on the palms and soles
Erythema and edema in the hands and feet
- Can also present as a lack of unwillingness to walk in toddlers (sometimes due to concurrent hip arthritis)
- In undiagnosed KD, can eventually present as periungual peeling that starts underneath the nail bed
Less likely KD if there is:
- Palatal petechiae (Staph or Strep infection)
- Exudative pharyngitis (Staph or EBV infection)
Expert opinion: Dr. Tremoulet also recommends sitting down with the parents to review any photos that they may have of their child over the preceding days. This can help you identify criteria that may have come and gone prior to presentation!
Images (from top left in clockwise order): Ocular injection with peri-limbic sparing, strawberry tongue, cervical lymphadenopathy, periungual peeling of feet, rash, and erythema of feet. Consent obtained from patients by the Kawasaki Disease Foundation and graciously shared with The Cribsiders.
Risk Factors for Kawasaki Disease
It is difficult to determine who is at greater risk for Kawasaki Disease since there is no mechanism or etiology fully known. Most of what is known is retrospectively established, but it includes the following groups are at a higher incidence of Kawasaki Disease or at higher risk for coronary aneurysms:
- Age < 6 months are at higher risk for CAAs (Salgado 2017)
- Extremes of anemia and platelet count (thrombocytopenia or thrombocytosis) can portend worse disease
- Earlier rise of inflammatory markers
- Self-identified race of patient and parents (in San Diego County; Tremoulet 2011)
- Editor’s Note: Race, even self-identified, is not an accurate surrogate for genetics. These may more accurately reflect the social determinants of health, shared communal exposures, and/or racist paradigms that place these patients at higher risk of not receiving adequate medical treatment (Boyd 2020).
Management of Kawasaki Disease
- Once confident in the diagnosis, give IVIG and initiate high-dose aspirin (30-50mg/kg/d divided q8 or q6)
- After 36 hours, monitor for recrudescence of fever
- If febrile after 36 hours, will need to give second-line therapy, which can include:
- IVIG (2nd dose increases risk of hemolytic anemia)
- Steroids
- Anakinra
- Infliximab
- Approved for Kawasaki Disease in Japan (but not in the US)
Upon Discharge
- Switch to intermediate- or low-dose aspirin after discharge
- If indicated, ensure that the patient is on the appropriate anticoagulation:
- If TTE Z-score ≥ 5 and < 10, consider dual antiplatelet therapy (with aspirin and clopidogrel)
- If TTE Z-score ≥ 10, therapeutic anticoagulation (e.g. enoxaparin) and low-dose aspirin
- Coordination of out-patient follow-up:
- Echocardiogram within one to two weeks post-discharge, which may require sedation
- Will need to determine when antiplatelet therapy can be discontinued
COVID-19, MIS-C, & Kawasaki Disease
It can be difficult to tell the difference between the two, and it is possible that there may be overlap between the two syndromes. If you need a refresher on MIS-C, see Episode #5 with Dr. Tremoulet! MIS-C tends to have more frequent follow-up due to their severe myocardial dysfunction.