Today I reviewed EM Quick Hits 38 ACS in Older Patients, Rural Neonatal Resuscitation, Hemophilia, Hiccups, ECG Computer Interpretation*,
*Helman, A. Shenvi, C. McLaren, J. Long, B. Ivankovic, M. EM Quick Hits 38 – ACS in Older Patients, Rural Neonatal Resuscitation, Hemophilia, Hiccups, ECG Computer Interpretation. Emergency Medicine Cases. May, 2022. https://emergencymedicinecases.com/em-quick-hits-may-2022/. Accessed 5-16-2022.
All that follows is from the above podcast and show notes.
Topics in this EM Quick Hits podcast
Christina Shenvi on ACS in older people (00:37)
Nour Khatib on rural NRP (11:40)
Jess McLaren on how not to get fooled by ECG computer interpretation (23:44)
Brit Long on hemophilia recognition and workup (30:10)
Maria Ivankovic on persistent and intractable hiccups from EM Cases Summit 2021 (36:20)
How not to miss ACS in older patients
- 65% of STEMIs and 80% of deaths from MIs occur in older patients
- The term “atypical” symptoms should be abandoned, as presentations of ACS without chest pain and presenting symptoms such as fatigue, weakness, dizziness and shortness of breath are common in older adults
- The most common presenting complaint in patients who have an MI who do not present with chest pain is dyspnea (followed by diaphoresis, nausea, vomiting and syncope)
- There are significant delays to assessment, obtaining ECG, diagnosis, treatment (i.e., delay to receiving ASA, longer door to PCI time) in older patients
- ECG interpretation is often more complicated in older patients who are more likely to have a pacemaker, ectopy, bundle branch blocks, LVH, dysrhythmias, atrial fibrillation, and pre-existing Q-waves
- Be proactive about obtaining and interpreting ECGs early and initiating treatment rapidly as these patients benefit from early PCI/fibrinolysis if it is within their goals of care
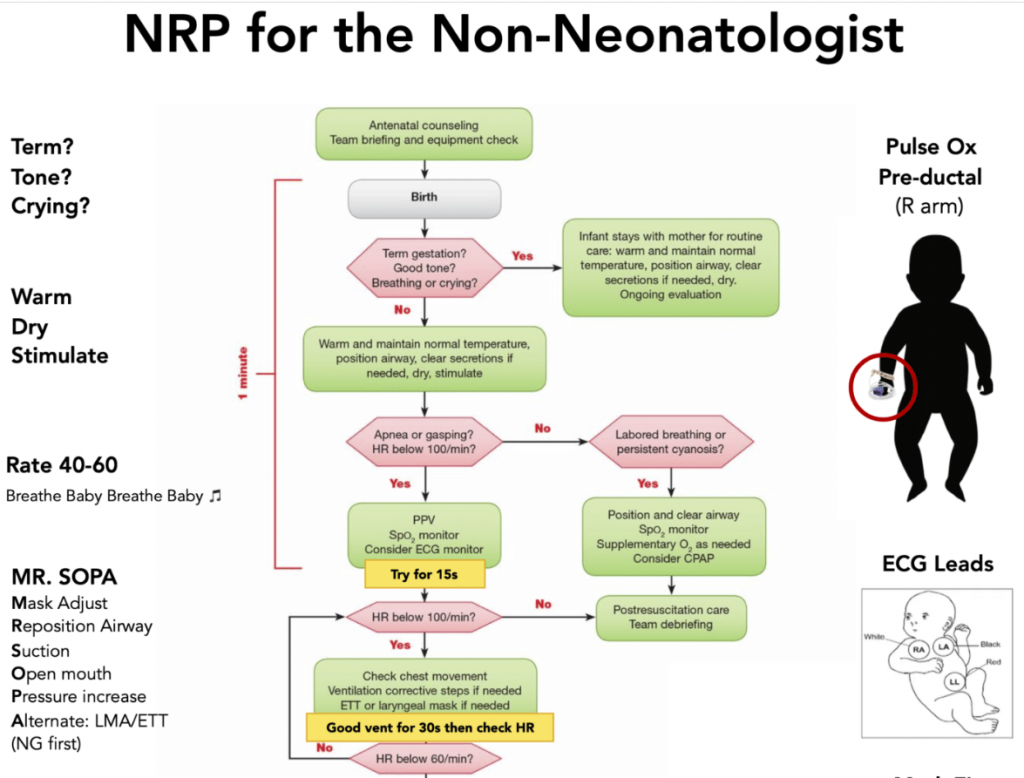
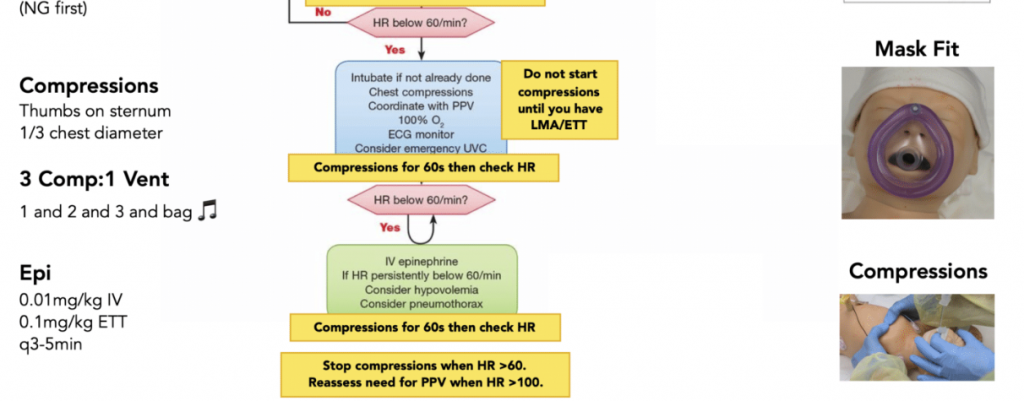
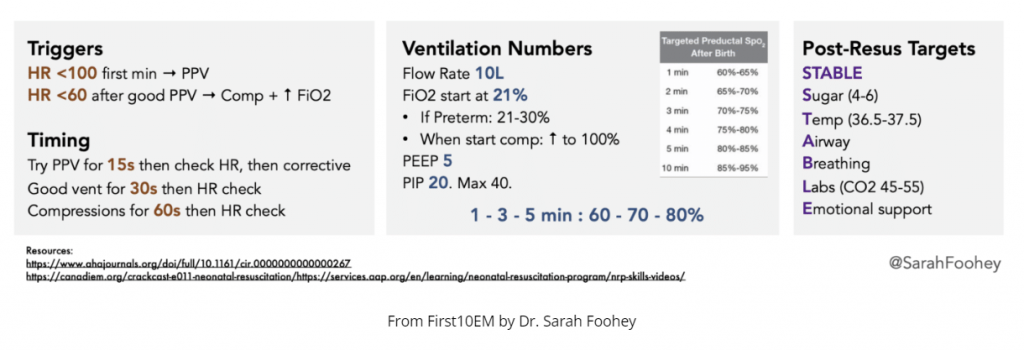
Practical tips for NRP in the ED/rural/remote settings
- Generally neonatal distress is caused by respiratory compromise and therefore resuscitation is ABC, not CAB
- Ensure equipment is prepared in advance: NRP algorithm on the wall, Miller zero and 1 blades, appropriately sized ET tubes, oxygen mask and BVM, smallest supraglottic airway, towels, plastic bag, umbilical vein catheter kit, scissors, clamp, IO
- Heat loss is a problem in premature babies; use the warmer, set to 25C, and put neonates <32 weeks GA in a plastic bag up to their neck without towel drying; target 36.5-37.5C
- Suctioning: nasopharyngeal and oral suctioning is no longer routinely recommended and is recommended only if there is airway obstruction; suction the mouth first and then the nose (think alphabetical order M-N)
- Monitors and positioning: place rolls under the shoulders, 3-lead ECG, SpO2 monitor, listen to the heart with stethoscope for HR, consider jaw thrust
- Positive Pressure Ventilation (PPV): avoid over-ventilation and pneumothoraces by using positive inspiratory pressures no greater than 20-25, give approximately 40-60 breaths per minute (can use the “breath-two-three, breath-two-three” recitation to achieve this)
- FiO2: it can take up to 10 minutes for a healthy newborn to reach an O2 saturation of 95%; do not jump to intubation if sats are in the 70s in the first minutes of life; start with FiO2 of 21%
- Supraglottic airway is the preferred advanced airway tool in neonates but cannot be used in premies <34 wks or 1.5kg as they are too large in this group
- Vascular access: for neonates <3kg an umbilical vein catheter is preferred access, IOs can be used in babies >3kg; medications such as epinephrine can be delivered down the ET tube if you cannot get vascular access
- Epinephrine dosing: UVC: 0.1mL/kg ET Tube: 1mg/kg
- Fluids: NS 10mL/kg over 20 minutes; glucose D10W 2mL/kg
Episode 142: Neonatal Resuscitation
Don’t be fooled! Tips for interpreting the computer ECG interpretation
When correct, the computer interpretation can improve physician accuracy, and when incorrect it increases error misdiagnoses and is estimated to account for approximately 10,000 adverse events/avoidable deaths per year. Experts suggest that learners should not look at the computer read-out initially, and should make their own interpretation first so as not to be misled by errors on the computer’s interpretation, while ECG experts can use the computer interpretation as a verification, or can correct it as needed.
Ten sources of ECG computer interpretation error:
ECG Acquisition: proper acquisition is important for interpretation; acquisition can be affected by:
- Motion Artifact: motion artifact produces a chaotic baseline (might be labelled as A-fib or polymorphic VT); see if you can map out regular R-waves through the noise, this can give you a clue that the rhythm is normal
- Limb lead reversal: can lead to inverted complexes, which produces a “pseudo-infarct” pattern in the inferior or lateral leads; clues include: inverted P-wave in lead I or II (opposite of sinus rhythm), entirely inverted P-QRS-T complexes or an abnormal axis
- Precordial lead reversal: can lead to a pseudo-infarct pattern in the anterior leads; the hint is that the R-wave progression is interrupted by an isolated abnormal lead
- Precordial lead misplacement: when V1 and V2 are too high on the chest, this can mimic anything from ST elevation (from Brugada or STEMI) to T wave inversion (from Wellen’s syndrome or pulmonary embolism), but the giveaway is that P-waves are normally biphasic in V1 and fully upright in V2, if V1 is fully negative, or V2 is biphasic or negative these leads are too high
Looking for proper acquisition: free from artifact, normal limb lead placement with upright P-wave in leads I and II , normal precordial lead placement with a biphasic P-wave in V1 and upright in V2, and a smooth R-wave progression without isolated abnormalities
Computer Interpretation/Measurement of ECG:
- Rate and rhythm: generally accurate in labeling normal sinus rhythm, high rates of error for other rhythms (deflections seen between QRS complexes can be P-waves, T-waves, U waves, flutter waves or artifact); best place to verify sinus activity is lead II where P-waves are upright or V1 where P-waves are biphasic
- Electrical conduction: generally good at measuring intervals, with some exceptions including short PR and delta waves in WPW which may not be present in all leads and could be missed, and prominent U waves which may lead to errors interpreting QT interval
- Axis: generally good at determining the axis, can not determine the cause of axis deviation
- R-wave progression: computer does not measure it, but is helpful to examine for loss of R-waves in an anterior MI or early R-wave progression in a posterior MI
- Voltage: often correctly labels low voltages but can’t correctly differentiate large amplitudes as LVH vs. early repolarization because they are often the same amplitude and we rely on other features to distinguish them
- ST segments and T-waves: computers can apply basic STEMI criteria, but these are neither sensitive nor specific; the computer cannot distinguish between primary, secondary or combination ST elevation, so it may label LVH a STEMI, while missing an occlusion MI in the presence of a LBBB, the computer also cannot identify other signs of occlusion MI that don’t meet classic STEMI criteria such as hyper-acute T-waves or reciprocal changes
ECG Cases 29: Misdiagnosis from Lead Misplacement, Artifact and Lead Reversal
ECG Cases 30: Beware Computer Interpretation Error
Hemophilia Part I – recognition and workup
- Hemophilia: bleeding disorder with a deficiency in one of the factors involved in the coagulation pathway, hemophilia A is a deficiency in factor VIII (80-85%); hemophilia B is a deficiency in factor IX; hemophilia C is a deficiency in factor XI
- Severity of hemophilia is based on the amount of available factor (factor level):
- Severe hemophilia: < 1 % factor available
- Moderate hemophilia: 1-5% factor available
- Mild hemophilia: 5-40% factor available
- Etiology:
- Hemophilia is most commonly an X-linked inherited disorder
- Other etiologies include spontaneous mutation (1/3 of cases) and an acquired form (autoantibodies)
- Females who carry the gene for hemophilia can also have low factor levels and are at risk of bleeding complications
- Severe hemophilia will present within first two years of life; think about hemophilia in:
- Pediatric patients with hemarthrosis
- Post circumcision bleeding
- Excessive or prolonged bleeding after small cuts and lacerations
- Bruises that are larger than what you would expect for the mechanism
- Also think about hemophilia in adult patients presenting with spontaneous bruising, mucosal bleeding, persistent menstrual bleeding, hematomas, subacute or delayed post-partum bleeding
- Categorize bleeding episodes as major and minor:
- Major bleeds: CNS, airway, eyes or orbits, nose, chest, GI tract, and retroperitoneum
- Minor bleeds: oral mucosa, joints, and muscles
- Hemarthrosis is the most common site, but the leading cause of death is intracranial bleeding
- History: bleeding site, mechanism, and whether they have a known diagnosis
- If known diagnosis, ask about the type of hemophilia, severity, prophylaxis and last factor replacement, prior bleeds, inhibitors, HIV and hepatitis C status, their emergency management plan, and if they have home factor with them
- Exam: CNS, HEENT, chest, GI, back/flanks/groin, musculoskeletal system
- Imaging: low threshold for imaging these patients
- Laboratory: CBC, coagulation panel, and factor activity level
- Classic lab findings: prolonged aPTT (normal PT, bleeding time, and platelet count)
- Pitfall: Laboratory and imaging should never delay factor replacement
- Pitfall: Imaging decision rules should not be used to determine need for imaging in patients with hemophilia
MASAC Document 257 – Guidelines for Emergency Department Management of Individuals with Hemophilia and Other Bleeding Disorders, 2019.