Today, I link to and excerpt from Emergency Medicine Cases‘ Ep 117 TIA Update – Risk Stratification, Workup and Dual Antiplatelet Therapy*.
* Helman, A, Himmel, W, Dushenski, D. TIA Update – Risk Stratification, Workup and Dual Antiplatelet Therapy. Emergency Medicine Cases. November, 2018. https://emergencymedicinecases.com/tia-update/. Accessed 6-13-2023.
*Also, see and review Helman, A, Himmel, W, Dushenski, D. ED Stroke Management in the Age of Endovascular Therapy. Emergency Medicine Cases. January, 2019. https://emergencymedicinecases.com/stroke-update-endovascular-therapy/. Accessed 6-13-2023.
All that follows is from Ep 117 TIA Update.
This is Part 1 of EM Cases two part podcast on TIA and Stroke with Walter Himmel and David Dushenski – TIA Update – Risk Stratification, Workup and Dual Antiplatelet Therapy.
Much has changed in recent years when it comes to TIA risk stratification, workup and antiplatelet therapy. In this podcast we use the overarching theme of timing to elucidate how to distinguish true TIA from the common TIA mimics, the importance of timing in the workup of TIA, why the duration of therapy with dual antiplatelet therapy and timing of starting anticoagulation in patient with atrial fibrillation, contributes to the difference between preventing catastrophic strokes and causing intracranial hemorrhage. Remember that stroke is a leading cause of adult disability and is the third leading cause of death in Canada. It’s time we paid more attention to TIA…
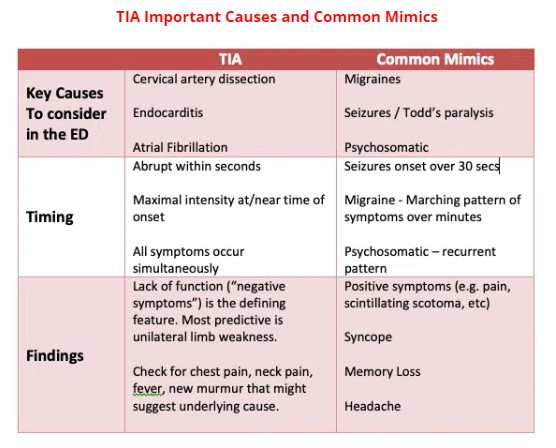
TIA Mimics
The ED misdiagnosis rate of TIA has been reported to be between 5% and 31%, which can lead to needless workups, iatrogenic complications and morbidity. The three mimics that are often not obvious on history and physical are migraines, seizures and psychiatric disorders. Distinguishing these from TIA is mostly in the timing of symptom onset, associated symptoms and presence of “positive” vs “negative” symptoms. It is important to consider a few of the less common underlying causes of TIA in the ED as these have time-sensitive workups and therapies.
An observational study from 2014 shows that memory loss, headache, and blurred vision were associated with mimics, while unilateral weakness was associated with true TIA.
Clinical Pearl: The “TIA AND” presentation. TIA symptoms AND neck pain – think neck dissection. TIA symptoms AND fever or new heart murmur – think endocarditis.
TIA risk stratification – the death of the ABCD2 score
The importance of risk stratification for TIA lies in the questions: what’s the chance that a TIA patient you see in the ED will have a stroke in the next 2 days? 90 days? And can we identify the patients who are eligible for a carotid endarterectomy fast enough to prevent that stroke?
There exists an alarming 12-20% 90 day stroke risk in those presenting with high risk TIA symptoms. Half of these patient suffer from a stroke in the first 48hrs. A 2016 NEJM study fortunately found that this high risk can be reduced to less than 4% with rapid follow-up and aggressive secondary prevention. Based on these findings, it is good practice for high risk TIA patients to be worked up in the first 48 hours.
So which patients who present with TIA symptoms are high risk?
While the CHADS2VASC helps identify AFib patients at risk for future embolic event, The ABCD2 score has been the most ubiquitously used risk stratifying tool in ED since its inception. The elements of the ABCD2 include:
- Age over 60
- Initial BP over 140/90
- Clinical features of unilateral weakness and speech impairment
- Duration of symptoms
- History of D
More recent studies by Stead and Ghia have failed to validate the ABCD2 score and have shown that the score is neither sensitive nor specific and is inaccurate, at any cut-point. In 2011, Perry’s external validation of the ABCD2 found that by using this score, physicians were misclassifying up to 8% of patients as low risk. Sensitivity of the score for high risk patients was found to be only 31.6%.
As recognized in the latest iteration of the Canadian Heart and Stroke Guideline from 2018, the most important prognostic feature of the ABCD2 score appears to be the Clinical features:
“Very High Risk for Recurrent Stroke (Symptom onset within last 48 Hours):
- Transient, fluctuating or persistent unilateral weakness (face, arm and/or leg);
- Transient, fluctuating or persistent language/speech disturbance;
- And/or fluctuating or persistent symptoms without motor weakness or language/speech disturbance (e.g. hemibody sensory symptoms, monocular vision loss, hemifield vision loss, +/- other symptoms suggestive of posterior circulation stroke such as binocular diplopia, dysarthria, dysphagia, ataxia).”
The bottom line: high risk patients are the ones with either true motor deficit of a limb or face or a speech deficit. This is important not only to determine who needs a rapid workup to assess eligibility for carotid endarterectomy and hopefully prevent a catastrophic stroke, but also to identify those patients who will likely benefit from dual antiplatelet therapy.
Update 2021: The Canadian TIA score was validated using a multicenter prospective cohort study involving 7607 patients in the ED with TIA or minor stroke, and was found to more accurately stratify the risk of subsequent stroke and carotid endarterectomy / stenting when compared to the ABCD2 and ABCD2i scores. Abstract