Also, see and review Large Vessel Occlusion Stroke Detection in the Prehospital Environment [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Curr Emerg Hosp Med Rep. 2021 Sep;9(3):64-72. doi: 10.1007/s40138-021-00234-9. Epub 2021 Jun 28
From the above abstract:
Purpose of review: Endovascular therapy for acute ischemic stroke secondary to large vessel occlusion (LVO) is time-dependent. Prehospital patients with suspected LVO stroke should be triaged directly to specialized stroke centers for endovascular therapy. This review describes advances in LVO detection among prehospital suspected stroke patients.
Summary: The use of a prehospital stroke severity tool for LVO triage is now widely supported. Ease of use should be prioritized as there are no meaningful differences in diagnostic performance amongst tools. LVO diagnostic devices are promising, but none have been validated in the prehospital setting. Mobile stroke units improve patient outcomes and cost-effectiveness analyses are underway.
Today, I link to and excerpt from Emergency Medicine Cases‘ Ep 120 ED Stroke Management in the Age of Endovascular Therapy*.
*Helman, A, Himmel, W, Dushenski, D. ED Stroke Management in the Age of Endovascular Therapy. Emergency Medicine Cases. January, 2019. https://emergencymedicinecases.com/stroke-update-endovascular-therapy/. Accessed 6-13-2023.
All that follows is from the show notes of the above resource.
According to the Global Burden of Disease Study published in NEJM in December 2018 the estimated lifetime risk for a 25 year old during their remaining lifespan is 25% [1]. Stroke is the 3rd leading cause of death and 1st leading cause of major disability in North America. As we transition from the relatively simple era of systemic thrombolytics under 3 hours vs “ASA and admit” for over 3 hours, decision making has become much more complicated and varied, depending on where you work. Which patients need what type of scanning? Where should that scanning be done – at the stroke center or at the peripheral center? Which patients should get systemic thrombolytics? Which patients should get endovascular therapy? In this EM Cases main episode podcast, a follow up to our episode on TIA released in November 2018 with Walter Himmel and David Dushenski, we try to simplify the confusing time-based and brain tissue-based options for stroke management…
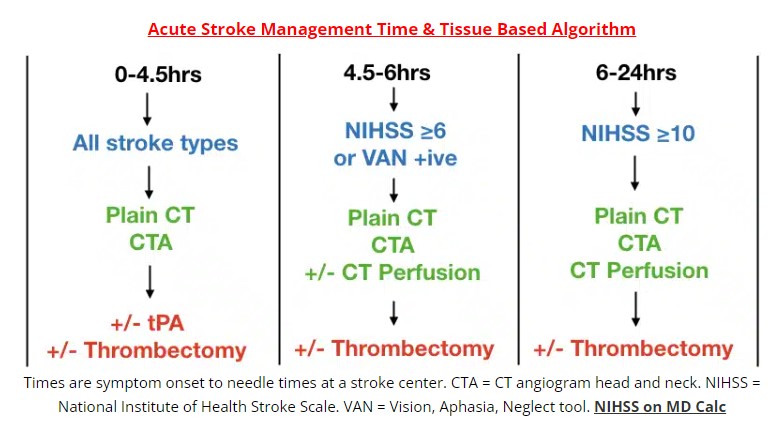
Time and image based stroke management algorithm
Activating a “code stroke” on every patient that experiences any acute neurologic event within 24hrs of symptom onset based on the DIFFUSE 3 and DAWN trials [2,3] may outstrip resources, with only a tiny minority of these patients receiving potential benefit. There is currently an effort to identify those patients clinically who might be most likely to benefit from endovascular therapy so that not all stroke patients require transport to a stroke center with multiple imaging modalities and resource-heavy acute stroke team care.
The workup and considerations for tPA and endovascular therapy (thrombectomy) depend on:
- Symptom onset to needle time
- Type of stroke, NIHSS or VAN tool (see below)
- CT, CT angiogram and CT perfusion results
- Contraindications to tPA/thrombectomy
Time is the key factor in patients with a symptom onset-to-needle time ≤ 6 hours.
Brain tissue salvageability determined by CT perfusion is the key factor in patients with a symptom onset-to-needle time of 6-24 hours.
In the 0-4.5 hours category, plain CT will rule in hemorrhagic stroke and CTA may diagnose an underlying vascular abnormality causing the bleed.
For patients in the 4.5-6 hours category, and with an NIHSS ≥6 or VAN positive, and plain CT and CTA consistent with cortical stroke, candidacy for thrombectomy is determined either by CT perfusion, or if CT perfusion is not readily available, by the ASPECTS score[6].
Update 2021: Retrospective cohort study across 1752 USA hospitals of 163,038 patients with acute ischemic stroke, either taking DOAC’s or not taking anticoagulants prior to stroke and treated with IV alteplase within 4.5 hours of symptom onset. Use of DOAC’s within the preceding 7 days, compared to no use of anticoagulants, was not significantly associated with increased risk of intracranial hemorrhage. Abstract 
Update 2022: A systematic review including 7 trials from 2012 to 2020 with 980 patients with “wake-up” strokes identified that 46% of patients who underwent endovascular thrombectomy had independent functional outcome (modified Rankin scale of 2 or less) compared to 9% of patients who were randomized to control (RR 5.12, 95% CI 2.57 to 10.17, P<0.001). The review also found that 66% of patients who underwent IV alteplase had functional outcome (modified Rankin scale of 2 or less) compared to 58% randomized to control (RR 1.13, 95% CI 1.01 to 1.26, P = 0.03). Abstract Using the VAN Tool to identify strokes that may be amenable to endovascular therapy
Which patients are most likely to benefit from endovascular therapy? Stroke patients with large vessel occlusions (“cortical stroke”) are the most likely to benefit from thrombectomy – internal carotid artery, MCA, and some ACA occlusions. An NIHSS ≥6 has traditionally been used to predict a cortical stroke. However this score is complicated and time consuming for the ED provider and ideally requires specific training to use it. Multiple prehospital prediction tools have been developed such as the LAMS and RACE , however their sensitivities for large vessel strokes were only in the 80’s. A more recent tool called the VAN tool (a mnemonic for Vision, Aphasia and Neglect) has been shown in a pilot study to have a 100% sensitivity and 90% specificity, 74% PPV and 100% NPV for large vessel stroke [7]. VAN was more specific than an NIHSS score ≥6 and just as sensitive for large vessel occlusion stroke. Although this study requires validation it is a promising tool to help us in the ED to identify clinically which patients should be considered for advanced imaging and endovascular therapy.