In this post I link to and excerpt from 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC [PubMed Abstract] [Full Text HTML] [Full Text PDF]. European Heart Journal (2020) 00, 1126.
All that follows is from the above resoure.
4 Epidemiology
Worldwide, AF is the most common sustained cardiac arrhythmia in adults10 (Figure 2, upper panel). AF is associated with substantial morbidity and mortality, thus portending significant burden to patients, societal health, and health economy (Figure 2, lower panel) (Supplementary section 1).
The currently estimated prevalence of AF in adults is between 2% and 4%,10 and a 2.3-fold rise11 is expected,12,13 owing to extended longevity in the general population and intensifying search for undiagnosed AF.15
5 Clinical features of atrial fibrillation
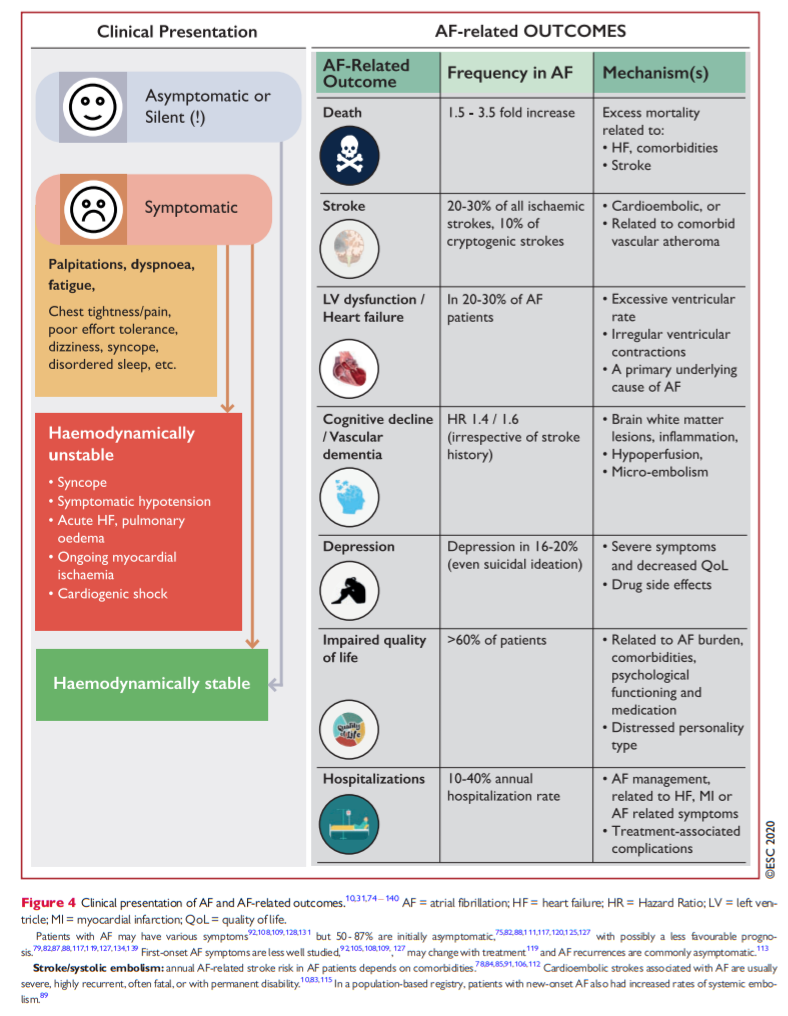
Clinical presentation of AF and AF-related outcomes are shown in Figure 4 (see also Supplementary section 2 and Supplementary Box 1).
6.1 Classification of atrial fibrillation
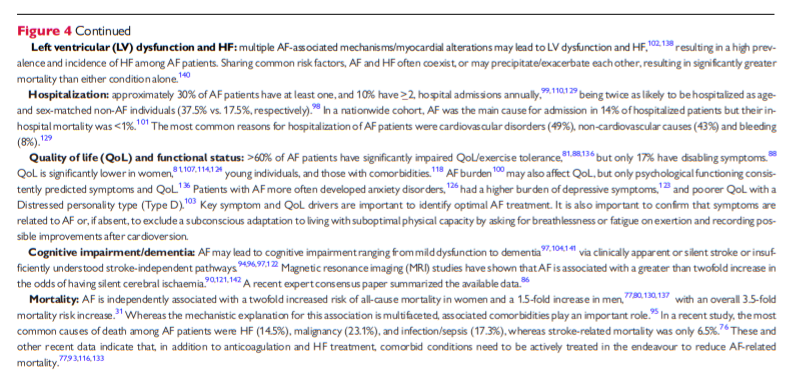
Different AF classifications have been proposed but, traditionally, five patterns of AF are distinguished, based on presentation, duration, and spontaneous termination of AF episodes (Table 4).143
10 Patient management: the integrated ABC pathway
The simple Atrial fibrillation Better Care (ABC) holistic pathway (‘A’ Anticoagulation/Avoid stroke; ‘B’ Better symptom management; ‘C’ Cardiovascular and Comorbidity optimization318) streamlines integrated care of AF patients across all healthcare levels and among different specialties. Compared with usual care, implementation of the ABC pathway has been significantly associated with lower risk of all-cause death, composite outcome of stroke/major bleeding/cardiovascular death and first hospitalization,319 lower rates of cardiovascular events,320,321 and lower health-related costs.322 In the prospective, randomized mAFA-II trial, the composite outcome was significantly lowered with ABC pathway management intervention compared with usual care [1.9% vs. 6.0%; hazard ratio (HR) 0.39; 95% CI 0.22 − 0.67; P <0.001].323
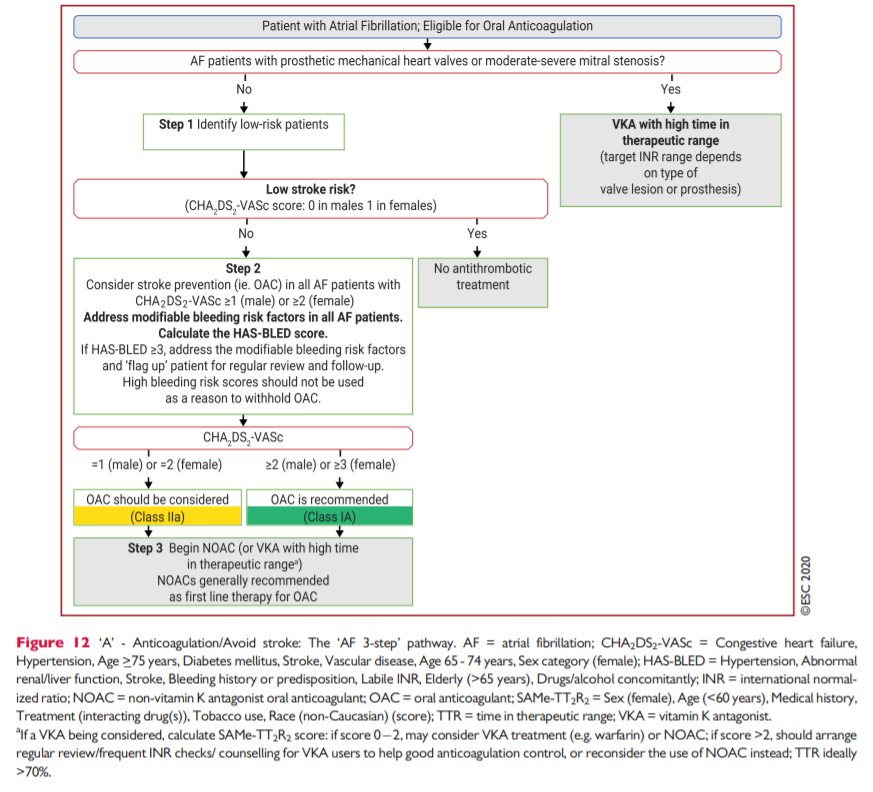
10.1.6 Decision making to avoid stroke
In observational population cohorts, both stroke and death are relevant endpoints, as some deaths could be due to fatal strokes (giventhat endpoints are not adjudicated in population cohorts, and cerebral imaging or post-mortems are not mandated). As OAC significantly reduces stroke (by 64%) and all-cause mortality (by 26%) compared with control or placebo,412 the endpoints of stroke and/or mortality are relevant in relation to decision making for thromboprophylaxis.The threshold for initiating OAC for stroke prevention, balancing ischaemic stroke reduction against the risk of ICH and associated QoL, has been estimated to be 1.7%/year for warfarin and 0.9%/year for a NOAC (dabigatran data were used for the modelling analysis).474 The threshold for warfarin may be even lower, if good-quality anticoagulation control is achieved, with average TTR>70%.475
Given the limitations of clinical risk scores, the dynamic nature of stroke risk, the greater risk of stroke and death among AF patients with >_1 non-sex stroke risk factor, and the positive net clinical benefit of OAC among such patients, we recommend a risk-factorbased approach to stroke prevention rather than undue focus on (artificially defined) ‘high-risk’ patients. As the default is to offer stroke prevention unless the patient is low risk, the CHA2DS2-VASc score should be applied in a reductionist manner, to decide on OAC or not.476
Thus, the first step in decision making (‘A’ Anticoagulation/Avoid stroke) is to identify low-risk patients who do not need antithrombotic therapy. Step 2 is to offer stroke prevention (i.e. OAC) to thosewith >_1 non-sex stroke risk factors (the strength of evidence differs, with multiple clinical trials for patients with >_2 stroke risk factors, and subgroups from trials/observational data on patients with 1 nonsex stroke risk factor). Step 3 is the choice of OAC—a NOAC (given their relative effectiveness, safety and convenience, these drugs are
generally first choice as OAC for stroke prevention in AF) or VKA (with good TTR at >70%). This ‘AF 3-step’ patient pathway182,477 for stroke risk stratification and treatment decision making is shown in Figure 12.