In this post, I link to and excerpt from Dr. Josh Farkas‘ Internet Book Of Critical Care [link is to the table of contents] chapter, Noninvasive Respiratory Support, Dec. 27, 2019.
Note to myself and my readers: Go to the link above and review the entire chapter directly in the IBCC. I only make the excerpts because it helps me fix the chapter in my memory.
All that follows is from the above resource.
CONTENTS
- Rapid Reference
- Groundwork:
- BiPAP & CPAP
- High flow nasal cannula (HFNC)
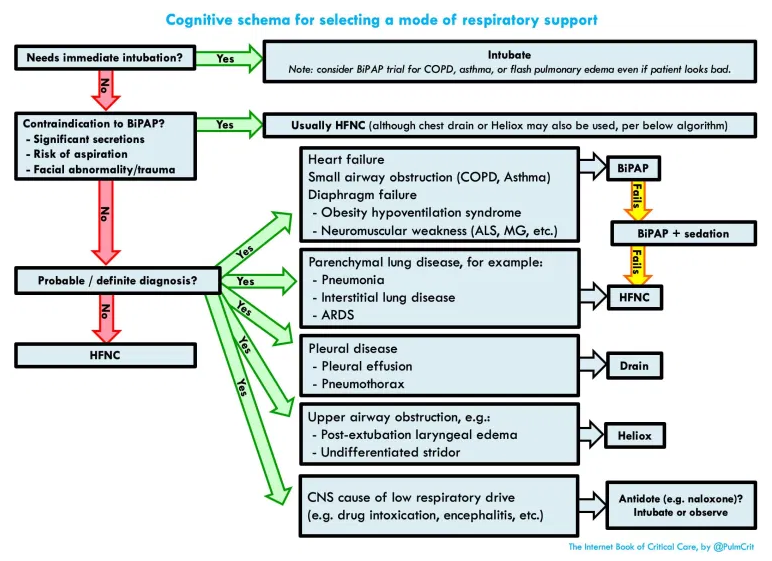
- Selecting which device to use
- Oxymizer
- Podcast
- Questions & discussion
rapid reference
goals & assessment
The goal of noninvasive respiratory support is essentially to support the patient long enough for other therapies to work (e.g. antibiotics, bronchodilators, steroids). This may take a bit of time. As long as the patient is comfortable, protecting their airway, and stable/improving, that’s OK.
appropriate goals for a patient receiving noninvasive respiratory support:
- Maintain adequate oxygenation.
- Provide adequate ventilatory support so that the patient is comfortable and doesn’t develop respiratory muscle fatigue.
- Allow for secretion clearance, if that is an issue (e.g. in pneumonia).
- The patient should be able to protect their airway from aspiration.
- Serial clinical evaluation should show that the patient’s condition is stable or improving.
inappropriate goals
- The patient must immediately improve.
- The ABG/VBG must immediately improve, or meet some arbitrary target (noting that such targets usually aren’t evidence-based).
- Some retrospective studies demonstrate that failure of the blood gas to improve correlates with a requirement for intubation. However, such studies are generally confounded because clinicians are utilizing these very same blood gas values as an indication for intubation! Thus, circular logic creates to a self-fulfilling prophecy.
- The patient must be able to be weaned off noninvasive respiratory support within a few hours.
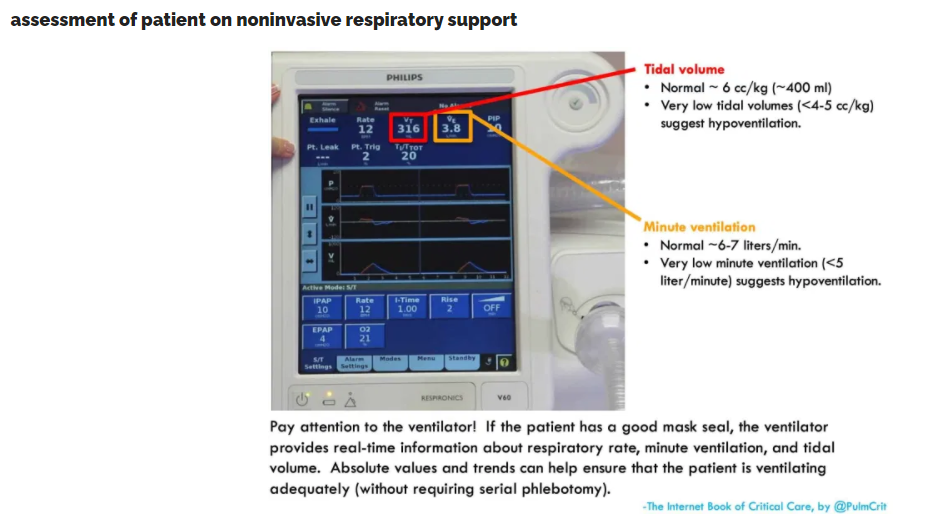
- Oxygenation should be adequate (e.g. >88%).
- If the patient has an reliable pulse oximetry waveform, this is the preferred assessment of oxygenation.
- To be clear: there are generally no advantages (and potentially some disadvantages) to using serial ABGs to assess oxygenation. ABGs should only be used if pulse oximetry is unreliable (e.g. due to a poor waveform or hemoglobinopathy).
- Work of breathing should be tolerable, and improved by noninvasive respiratory support.
- Respiratory rate trends are extremely useful.
- Other examination findings may reflect work of breathing (retractions, tri-podding, ability to speak in sentences, the patient’s perception of their breathing).
- Global overall appearance (including mentation)
- How does the patient look?
- As long as the patient is mentating normally, their PaCO2 isn’t profoundly elevated.
- When in doubt, frequent re-assessment will often clarify the patient’s trajectory. Discussion with other team members (e.g. nurse and respiratory therapist) can help enormously.
- ABG/VBG?
- These are generally not needed. If the other parameters are reassuring (i.e. oxygenation, work of breathing, appearance, mentation), then an ABG/VBG is unnecessary. Alternatively, if the patient is deteriorating clinically, then a normal ABG shouldn’t be reassuring.
- The main indication for blood gas analysis is if the patient’s mental status is abnormal, but it’s unclear whether mental status is altered due to hypercapnia or medication (e.g. patients receiving sedation to tolerate the BiPAP).
- Venous blood gas is entirely adequate in nearly all cases (unless the VBG oxygen saturation is incredibly low).
Please note, review the entire chapter.