In this post, l link to and excerpt [from When Do We Need EEG Monitoring In Critical Care] From Dr. Farkas‘ IBCC [Link to TOC] Chapter “EEG interpretation and ictal-interictal continuum“, June 13, 2022.
All that follows is from the IBCC chapter above.
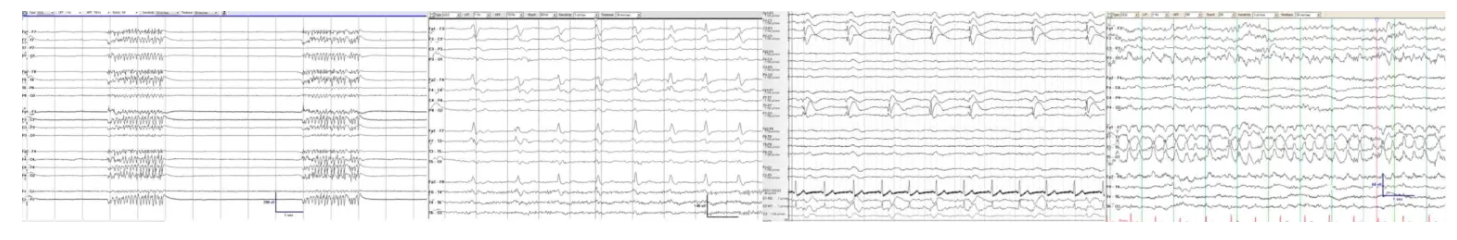
EEG is an increasingly utilized tool among critically ill patients. This chapter explores how to interpret the clinical significance of various EEG patterns which are commonly encountered in the ICU.
CONTENTS
- When & how long to monitor EEG:
indications for EEG monitoring in the ICU
There is a broad variety of indications for EEG monitoring in the ICU (e.g., for any patient in whom there is a concern for nonconvulsive status epilepticus – as discussed further here). Thus, the decision to pursue EEG monitoring is a complex one, which will often involve neurology consultation. Below are some rough guidelines (which are not intended to replace expert judgement).
general rationale
- Seizures or nonconvulsive status epilepticus are commonly detected among ICU patients (including “medical” or “surgical” ICU patients).(LaRoche 2018) Recognition of seizures is generally important for two reasons:
- (1) Seizures may impair consciousness, thereby clouding neuroprognostication and delaying recovery/rehabilitation.
- (2) Nonconvulsive status epilepticus may directly cause neurological injury (constituting one mechanism of secondary injury that can exacerbate critical neurologic illnesses).
- EEG monitoring is safe, so the main drawback is that it incurs some cost. However, by facilitating more rapid recovery and extubation, EEG monitoring may be cost-neutral or cost-saving.
indications for prolonged EEG monitoring (34618762)
- Persistently abnormal mental status after generalized convulsive status epilepticus or clinically evident seizure(s).
- A postictal period is expected following seizure(s), but this should usually clear within an hour.(LaRoche 2018) Persistent alteration of mental status suggests the possibility of ongoing seizure activity.
- Nonconvulsive status epilepticus is commonly encountered following convulsive status epilepticus. However, nonconvulsive status epilepticus can occur following only a single convulsive seizure.
- Assessment of treatment efficacy in patients with known status epilepticus (e.g., titration of antiepileptic infusions to target absence of seizures or burst-suppression).
- A screening (“spot”) EEG has revealed patterns along the ictal-interictal continuum, which increase the likelihood of subsequent seizures.
- Paroxysmal clinical events suspected to be possible seizures.
- Patients at risk for seizures which may be masked by the requirement for pharmacologic paralysis.
- Fluctuating mental status or unexplained alteration of mental status.
- Nonconvulsive status epilepticus or subclinical seizures occur in ~15% of critically ill patients with encephalopathy, even in the absence of acute brain injury (i.e., medical or surgical ICU patients).(34798964)
- This includes patients with acute supratentorial brain injury whose mental status is worse than would be expected.
- Comatose patients following cardiac arrest.
duration of EEG monitoring
sensitivity of EEG for seizure increases with longer duration of monitoring
- A single “spot” EEG recording over an hour may have only ~50% sensitivity for detecting seizure, as compared to ongoing continuous EEG monitoring. Increasing monitoring for 24-48 hours further increases sensitivity.
- Beyond a certain duration, the value of ongoing EEG monitoring becomes murky. For example, if the patient is having a subclinical seizure every 30 hours, does that truly matter? Would treating such an abnormality lead to more benefit than harm? This is unknown in the context of critical illness (wherein seizures may often improve over time merely due to treatment of the underlying disorder).
continuous versus spot EEG (aka “screening EEG”)
- Continuous EEG has greater sensitivity for seizures, but this comes at increased cost. Additionally, a hospital has only a limited number of EEG machines available. Consequently, it is important to determine which patients truly require continuous EEG monitoring.
- As a rough rule of thumb: If the following criteria are met, a short EEG recording may be sufficient to exclude seizures with reasonable sensitivity:(31886441)
- (1) Lack of prior seizure history.
- (2) No ongoing coma.
- (3) EEG recording reveals no worrisome findings (e.g., lateralized periodic or rhythmic delta activity).
- The 2HELPS2B algorithm (below) provides a more sophisticated and evidence-based approach for determining which patients require extended EEG monitoring.
2HELPS2B risk score for predicting electrographic seizures
- 2HELPS2B is a validated algorithm that predicts the risk of seizures based on clinical information combined with an initial 1-hour screening EEG. This helps determine how long it is appropriate to monitor the patient on EEG (e.g., a lower score would support more prompt discontinuation of EEG monitoring).
- Components of algorithm:
- 1 point each:
- Frequency >2 Hz for any periodic or rhythmic EEG pattern (except for GRDA).
- Epileptiform discharges (sporadic).
- Lateralized pattern (LRDA, LPD, BIPD).
- “Plus” features (including superimposed rhythmic, fast, or sharp activity).
- Seizure history, or recent events suspicious for clinical seizures.
- 2 points: BIRDS
.
- Risk of seizure:
- 0 points: ~3-4%
- 1 point: ~12%
- 2 points: ~27%
- 3 points: ~50%
- 4 points: ~73%
- 5 or more points: ~88%
- Implications of the duration of EEG monitoring (noting that clinical judgement is also involved):
- 0 points: Screening EEG alone may be adequate.
- 1 point: 12 hours of EEG screening may exclude seizure with ~95% sensitivity.
- 2 points: 24 hours of EEG screening or more may be needed if the goal is detection of >95% of all seizures.
- Limitations:
- (1) This is all based on an initial EEG recording of one hour (which may be longer than the duration of a spot EEG at many centers).
- (2) This may be confounded by sedative/anesthetic agents on board during the screening EEG.
- (3) The “prescription” for duration of EEG monitoring doesn’t take into account the findings during ongoing EEG monitoring. For example, imagine that a patient has a 2HELPS2B score of “1” and is subsequently found to have BIRDs during their 12-hour continuous EEG – that patient would undoubtedly warrant ongoing monitoring for >12 hours.
- Basics
- EEG in encephalopathy/coma
- Seizures
- Ictal-Interictal continuum
- Other abnormalities
- Podcast
- Questions & discussion
- Pitfalls