Dr. Horeczko’s podcast, Adventures in RSI [link is to show notes and podcast], from Pediatric Emergency Playbook is an outstanding review of everything important to consider in Pediatric Rapid Sequence Intubation. You really want to review the podcast and show notes more than once.
At the end of the post Dr. Horeczko summaries his talk as follows:
In summary, in these cases of sepsis, multitrauma, cardiogenic shock, and status epilepticus:
- Resuscitate before you intubate
- Use the agent’s specific properties and talents to your benefit
- Adjust the dose in critically ill patients: decrease the sedative, increase the paralytic
- Have post-intubation care ready: analgesia, sedation, verification, NG/OG/foley
Dr. Horeczko presents and discusses four cases:
-
Case 1 from 0 to 23:30 is about a 2 month old with bronchiolitis and likely viral sepsis who is in impending cardiovascular collapse. She is in respiratory failure and she needs her airway taken over but is she stable enough for intubation? Dr. Horeczko states “We have a few minutes to optimize, to resuscitate before we intubate.” [We remember that RSI in an unstable patient can lead to cardiovascular collapse. So we will give this patient fluid boluses and if forced to intubate before fluid boluses have kicked in perhaps a push dose pressor. For information on pediatric pulse dose pressors, see Another Great YouTube Video from Dr. Mellick–Pediatric Pulse Dose Pressor Administration Posted on October 2, 2014 by Tom Wade MD.]
-
Case 2 from 22:30 to 29:10 is the case of multiple trauma in a 3 year old boy. Dr. Horeczko discusses the considerations on what induction agent and what paralytic agent we should use in this trauma patient. “We need to adjust our dosing for a critically ill patient: Decrease the sedative to avoid falling over the hemodynamic compensation cliff. Increase the paralytic to account for prolonged arm-brain time.”
-
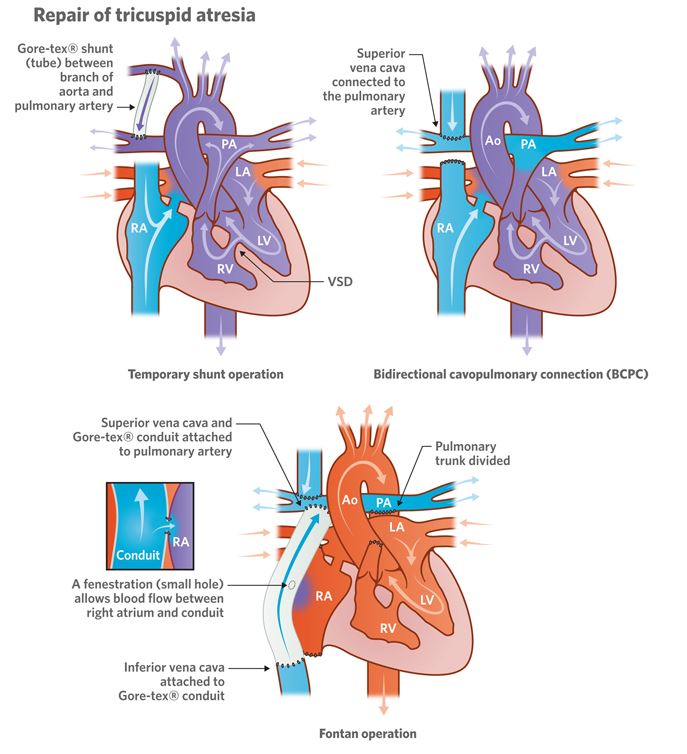
Case 3 from 29:10 to 40:35 discusses Cardiac/myocarditis/congenital heart disease. “Jacob is a 6-year-old-boy with tricuspid atresia s/p Fontan procedure who’s had one week of runny nose, cough, and now 2 days of high fever, vomiting, and difficulty breathing. “The Fontan procedure is the last in a series of three palliative procedures in a child with complex cyanotic congenital heart disease with a single-ventricle physiology. “The procedure reroutes venous blood to flow passively into the pulmonary arteries, because the right ventricle has been surgically repurposed to be the systemic pump. The other most common defect with an indication for a Fontan is hypoplastic left heart syndrome. “Typical “normal” saturations for post-operative CHD can be 75 and 85% on RA. The Fontan procedure improves saturations, which are typically 88-95%. Ask the parents or caregiver.
 ” A patient with a Fontan can present in cardiogenic shock from heart failure, distributive shock from an increased risk of infection, hypovolemic shock from over-diuresis or insensible fluid loss – or just a functional hypovolemia from the fact that his venous return is all passive – and finally obstructive shock due to a pulmonary thromboembolism.” Dr. Horeczko gives a great discussion on the use of fluids and pressors in these kind of cases.” “Induction Agent in Cardiogenic Shock: A blue baby – with a R –> L shunt – needs some pinking up with ketamine A pink baby – with a L –> R shunt – is already doing ok – don’t rock the boat – give a neutral agent like etomidate.” “Myocarditis or other acquired causes of cardiogenic shock – etomidate. Ketamine is an acceptable alternative, but watch for tachydysrythmias.” [See also Dr. Helman’s outstanding podcasts EMC Episode 84 – Congenital Heart Disease Emergencies and his EMC Best Case Ever 47 – Cyanotic Infant and Congenital Heart Disease Rx – Pre + Post Repair From Dr. Elizabeth Weinstein Posted on August 28, 2016 by Tom Wade MD]
” A patient with a Fontan can present in cardiogenic shock from heart failure, distributive shock from an increased risk of infection, hypovolemic shock from over-diuresis or insensible fluid loss – or just a functional hypovolemia from the fact that his venous return is all passive – and finally obstructive shock due to a pulmonary thromboembolism.” Dr. Horeczko gives a great discussion on the use of fluids and pressors in these kind of cases.” “Induction Agent in Cardiogenic Shock: A blue baby – with a R –> L shunt – needs some pinking up with ketamine A pink baby – with a L –> R shunt – is already doing ok – don’t rock the boat – give a neutral agent like etomidate.” “Myocarditis or other acquired causes of cardiogenic shock – etomidate. Ketamine is an acceptable alternative, but watch for tachydysrythmias.” [See also Dr. Helman’s outstanding podcasts EMC Episode 84 – Congenital Heart Disease Emergencies and his EMC Best Case Ever 47 – Cyanotic Infant and Congenital Heart Disease Rx – Pre + Post Repair From Dr. Elizabeth Weinstein Posted on August 28, 2016 by Tom Wade MD] -
Case 4 is from 40:35 to of a pt in status epilepticus. “Jessica is a 10-year-old girl with Lennox-Gastaut syndrome who arrives to your ED in status epilepticus. She had been reasonably controlled on valproic acid, clonazepam, and a ketogenic diet, but yesterday she went to a birthday party, got into some cake, and has had stomach aches – she’s been refusing to take her medications today. “On arrival, she is hypoventilating, with HR 130s, BP 140/70, SPO2 92% on face mask. She now becomes apneic.” “Induction Agent in Status Epilepticus: Many choices, but we can use the properties of a given agent to our advantage. She is normo-to-hypertensive and tachycardic. She has been vomiting. A nice choice here would be propofol. Propofol as both a sedative and anti-epileptic agent works primarily on GABA-A and endocannabinoid receptors to provide a brief, but deep hypnotic sedation. Side effects can include hypotension, which is often transient and resolves without treatment. Apnea is the most common side-effect. Ketamine would be another good choice here, for its anti-epileptic activity. We preoxygenate using apneic oxgygen at 10 liters/min [for adults we use 15 liters/min, school-age children 10 liters/min, and for infants and toddlers 5 liters/min].” “Paralytic Agent in Status Epilepticus: Rocuronium (in general), as there are concerns of a neurologic comorbidity.” “For ongoing pain and sedation we can start a midazolam drip and a fentanyl drip. I like to give a bolus of fentanyl initially [at the time of the propofol induction] because we know that we can’t sedate people out of pain. And of course propofol doesn’t have any analgesic effects.”




