In this post, I reviewed the Cubsiders’ Von Willebrand Disease episode*.
*Mao C, Weyand A, Lee N, Masur S, Chiu C, Berk J. “#64: Von Willebrand Disease.” The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ September 21, 2022.
All that follows is from the outstanding show notes.
Learning objectives
After listening to this episode listeners will…
- Take a thorough bleeding history and identify red flags.
- Explain the basic pathophysiology of von Willbrand disease and its effect on hemostasis.
- Be familiar with the diagnostic criteria of von Willebrand disease and its subtypes.
- Describe the role of desmopressin, von Willebrand factor concentrate, and antifibrinolytics in treatment and prophylaxis.
Von Willebrand Disease Pearls
- Have a low index of suspicion to test for VWD because it is the most common bleeding disorder (found in 1-2% of the population).
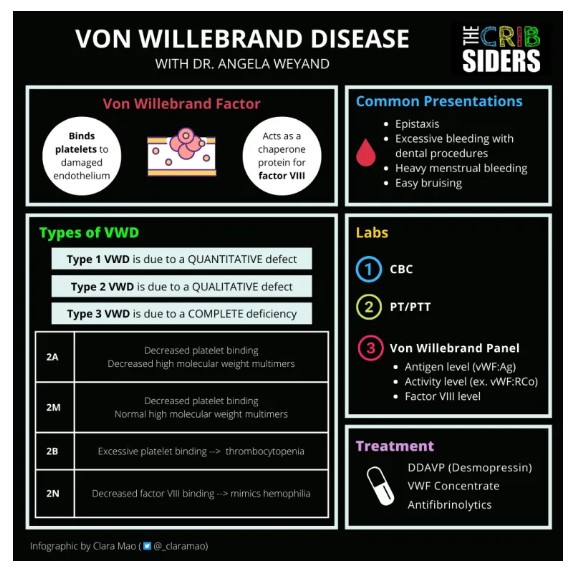
- Common presentations of VWD include epistaxis, bleeding with dental procedures, heavy menstrual bleeding, and easy bruising.
- Remember that many factors can falsely elevate VWF levels, including estrogen (ex. use of OCPs), stress/anxiety (ex. crying toddlers, acute illness, active bleeding), and exercise.
- Labs to check when evaluating for VWD include a CBC, PT/PTT, factor VIII level, VWF:Ag (antigen level), and VWF:RCo or VWF:Gp1b (activity level).
- Diagnosis of von Willebrand Disease is made when VWF level (either antigen or activity) is <30% regardless of bleeding history or <50% with a bleeding history.
- Type 1 VWD is due to a quantitative defect, meaning that there should be a symmetric decrease in activity level relative to antigen level (activity to antigen ratio >0.7).
- Type 2 VWD is due to a qualitative or functional defect, meaning that there is a significantly less activity level for a given antigen level (activity to antigen ratio <0.7).
- Treatment and prophylaxis options include desmopressin, VWF concentrate, and antifibrinolytics.
What is von Willebrand Factor?
Von Willebrand factor is a glycoprotein that plays a role in both primary and secondary hemostasis. In primary hemostasis, it binds platelets to exposed collagen on damaged endothelium in order to form the primary platelet plug. In secondary hemostasis, it acts as a chaperone protein for factor VIII to prevent it from being degraded too rapidly.
There can be significant variability in the presentation of VWD, even in patients with similar laboratory findings. Patients frequently report mucocutaneous bleeding including epistaxis, bleeding with dental procedures, easy bruising, or heavy menstrual bleeding. Those with more severe disease may also have muscle/joint bleeding or GI bleeding.
How to Take a Bleeding History
When taking a bleeding history, Dr. Weyand suggests going from head to toe:
- Does your child get nosebleeds? How long do they last? Are they unilateral or bilateral?
- Any excessive bleeding with dental procedures (ex. teeth extractions) or eruption of teeth?
- Have they had bruising in abnormal locations or larger than the size of a quarter?
- What about blood in the urine or stool?
- Do they have heavy periods? (for more information on how to take a menstrual history, check out our episode on Heavy Menstrual Bleeding)
The Self-Bleeding Assessment Tool is also an excellent screening tool that can be completed by patients in clinic.
Types of von Willebrand Disease
Type 1 (autosomal dominant): This is the most common type of VWD and is found in 70-80% of patients. Type 1 disease is due to a quantitative defect. VWF binds platelets and collagen normally, there just isn’t enough of it. Usually causes mild bleeding.
- Type 1C – Premature clearance of VWF
Type 2 (autosomal dominant): Type 2 disease is due to a qualitative/functional defect.
- Type 2A – Defect in platelet binding related to loss of high molecular weight multimers
- Type 2M – Defect in platelet binding but normal high molecular weight multimers
- Type 2B – Excessive binding to platelets leading to premature clearance and thrombocytopenia
- Type 2N –Decreased binding of factor VIII (can mimic hemophilia)
Type 3 (autosomal recessive): Most severe and <1% of all cases. In these patients, there is a complete deficiency of VWF.
Labs
When concerned about a possible bleeding disorder, start by checking:
- CBC – to evaluate for anemia and thrombocytopenia (don’t want to miss ITP)
- PT/PTT – to screen for factor deficiencies (note: this can be tricky because viral illnesses can cause kids to have transient lupus anticoagulant antibodies that falsely increase PTT and because PTT may not be prolonged for very mild factor deficiencies)
Von Willebrand Panel
The von Willebrand panel usually includes three components:
- Factor VIII level
- Antigen level (VWF:Ag) – amount of VWF in circulation
- Activity level (VWF:RCo or VWF:GP1b) – assess function of VWF through a platelet binding assay using ristocetin cofactor or GP1b
Diagnosis of von Willebrand Disease is made when VWF level (either antigen level or activity level) is <30% regardless of bleeding history, or <50% with a bleeding history.
To determine if a patient has type 1 or type 2 disease, compare the ratio of VWF activity level to VWF antigen level.
- If the ratio is >0.7, then the patient has type 1 VWD (symmetric decrease in activity and antigen levels)
- If the ratio is <0.7, then then the patient has type 2 VWD (significantly less activity level for given antigen level due to functional defect)
Expert Opinion: If referring a patient to hematology, Dr. Weyand suggests NOT checking a von Willebrand panel beforehand because they are best drawn, run, and interpreted in centers with specialized hematology labs (Brown et al 2021).
Treatment
Most patients with von Willebrand disease will only need episodic treatment for active bleeding and prophylaxis before procedures.
Desmopressin (DDAVP)
Causes release of endothelially stored VWF and can be used to treat minor bleeding or to increase levels prior to minor procedures. Patients should first undergo a desmopressin trial because there can be variability in response to the medication. Works best for type 1 disease because the factor released in type 2 disease is still functionally impaired. Contraindicated in type 2B disease because it can cause thrombocytopenia and in type 3 disease because of lack of efficacy. Was previously available outpatient in intranasal form, but is now only found as an IV medication (Connell et al 2021).
- Note: Important to instruct families about fluid restriction to decrease risk of hyponatremia.
VWF Concentrate
Used to treat major bleeding or as long-term prophylaxis for patients with severe recurrent bleeding. This includes patients with type 3 disease who are at high risk for hemarthrosis and patients who have significant GI bleeding (Connell et al 2021).
- Note: Comes in plasma and recombinant forms with and without factor VIII. Be aware that high factor VIII levels can increase risk of thrombosis.
Antifibrinolytics
Available in liquid, intranasal, and topical forms to use as adjunctive treatment or prophylactic therapy. Especially helpful for mucocutaneous bleeding (ex. epistaxis, heavy menstrual bleeding, oral bleeding).
Counseling
Dr. Weyand reminds us of key points to counsel families of patients with VWD about:
- Patients need surgical clearance for ANY dental procedure, including teeth extractions
- Encourage patients to wear a medical alert bracelet in case of emergency
- Consider screening siblings of patients with VWD before significant procedures (ex. tonsillectomy)
- Participation in football, boxing, and hockey should be avoided because of the risk of brain bleeding
- Think twice before using NSAIDs because of their antiplatelet effects BUT it is reasonable to consider occasional use in patients with dysmenorrhea