In addition to the article referenced in this post, be sure review Resources 2 through 5 in Resources below (all are from the article discussed in this post). These additional resources discuss periprocedural management of anticoagulated patients [2], balancing stroke and bleeding risk in AF patients [3], duration of dual antiplatelet therapy in CAD [4], and prevention of bleeding in patients with atrial fibrillation undergoing PCI [5].
What follows are excerpts from 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants:
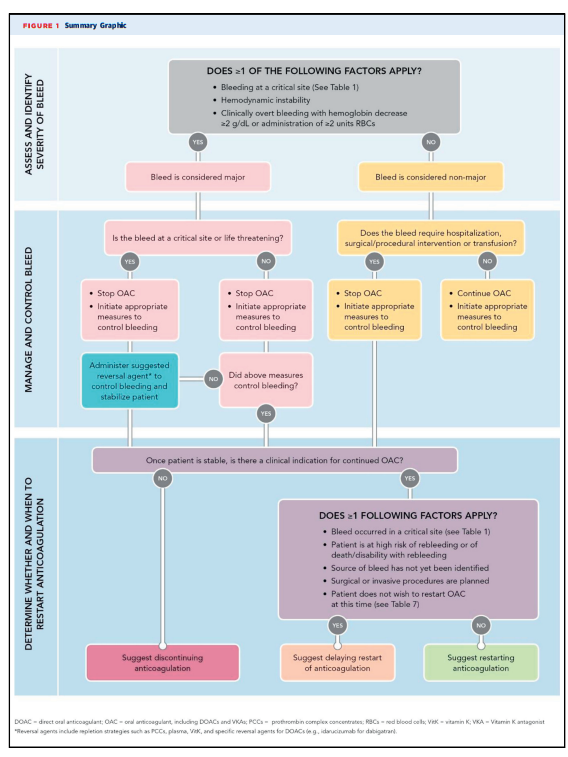
The article contains six figures and nine tables that excellently summarize the points and I’ve included them in this post. However, the article text needs to be reviewed completely. I have included some excerpts from the text.
1. INTRODUCTION
The guidance in this document is designed to address the clinical problem of bleeding management of patients treated with anticoagulants and will consider both DOACs and VKAs used for any indication. The decision pathway considered the severity of the bleed (major vs. nonmajor), acute medical and surgical management, the need for reversal, the appropriateness and time of restarting anticoagulation, and the impact of pertinent comorbidities and concomitant drug therapy. At each step in the decision pathway algorithms, patient specific factors should be considered.
2. METHODS
This decision pathway focuses on the management of bleeding in patients being treated with DOACs and VKAs for any indication. The role and management of antiplatelet agents is considered in the treatment algorithms. Bleeding classification has been simplified and is categorized as major or nonmajor (9). The former includes bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion (greater than or equal to2 U of packed red blood cells [RBCs]) or results in a hemoglobin drop of greater than or equal to 2 g/dL. All other bleeding is categorized as nonmajor. The recommendations provided by this decision pathway include guidance for temporary or permanent interruption of therapy, general approaches to bleeding management, decision support for treatment with a reversal agent, and indications and timing for reinstituting anticoagulant treatment.
The primary goal of this decision pathway is to guide the management of acute bleeding in patients treated with oral anticoagulants (OACs) and to supplement the 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Non-Valvular AF [Resource 2, below] , which addresses the management of patients undergoing planned surgical or interventional procedures.
3.1. General Clinical Assumptions
1. The pathway considers acute bleeding in patients being treated with either DOACs or VKAs.
2. In the setting of bleeding with hemodynamic compromise, standard resuscitative measures should always be performed promptly.
3. All indications for anticoagulation were considered, including AF, venous thromboembolism treatment and prevention, prosthetic cardiac valves, history of prior thromboembolism, intracardiac thrombus, and the presence of a mechanical cardiac support device (e.g., left ventricular assist device).
4. The recommendations for restarting and withholding anticoagulant therapy refers to both DOACs and VKAs.
5. The pathway algorithm assumes that the provider will seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible.