Another serious cause of headache and/or neurologic change is cerebral venous thrombosis which is diagnosed with MR venography or CT venography. See Links To And Excerpts From “European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis – Endorsed by the European Academy of Neurology”
Posted on December 30, 2023 by Tom Wade MD
Today, I review, link to and excerpt from The Cribsiders’ #81: Pediatric Brain Tumors – Let’s Think About It!* March 29, 2023 | By Sam Masur.
*Holloway R, Hummel T, Lee N, Mao C, Masur S, Chiu C, Berk J. “#81: Pediatric Brain Tumors – Let’s Think About It!”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ March 29, 2023.
All that follows is from the above resource.
Summary:
Brain tumors can be intimidating, for families and providers alike! Tune into this episode as Dr. Trent Hummel, Pediatric Neuro-Oncologist, guides us through the red flags to look for, when to escalate care and how to approach discussions with families. This conversation will blow your mind!
Pediatric Brain Tumor Pearls
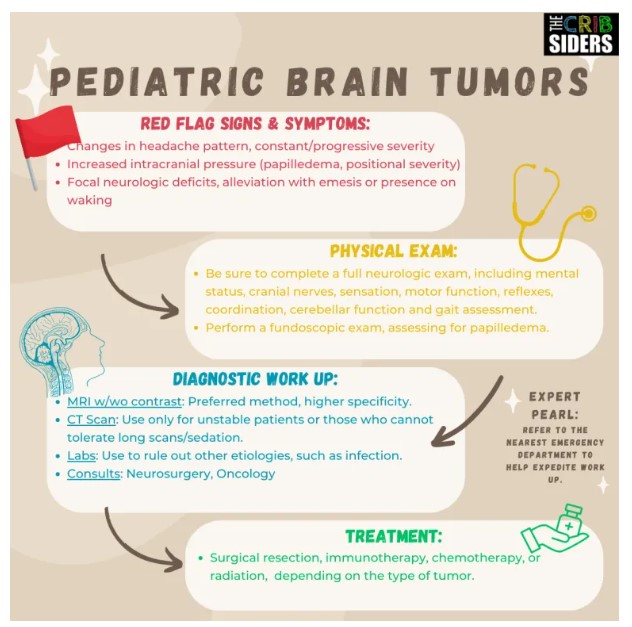
- When a patient presents with headache, be on the lookout for red-flag signs and symptoms, including severe and sudden onset, persistent and progressive pain, pain upon waking in the morning, alleviation of pain with vomiting or new-onset neurologic symptoms (frequent falls, dizziness, lack of use of an extremity, etc.).
- In addition to obtaining a symptom history, be sure to take a thorough past medical history, medication reconciliation and social history, looking for pertinent factors such as smoking or drug use.
- Complete a thorough neurologic and fundoscopic exam in patients with red flag symptoms.
- If you have concern for a potential mass-like process, you should have a low threshold for obtaining imaging. CT scans are good for screening, and MRIs are more definitive. Take into consideration your patient’s individual factors (ability to tolerate longer scans, ability to undergo sedation, etc.) and your level of concern in deciding which imaging is best.
- Obtain lab work judiciously – consider a complete blood count and a renal panel to assess for anemia/leukocytosis and electrolyte abnormalities, respectively.
- In cases in which you have high concern for a brain mass, consider referring to an Emergency Department to expedite work up.
- The majority of pediatric brain tumors are in the posterior fossa (60%). The most common types, in decreasing frequency, include medulloblastoma, juvenile pilocytic astrocytoma (JPA), ependymoma, diffuse intrinsic pontine glioma (DIPG), and atypical teratoid rhabdoid tumor (ATRT). The other 40% of pediatric brain tumors are in the cerebral hemispheres of the brain, and include astrocytomas, gangliogliomas, craniopharyngiomas and meningiomas, amongst others. [1]
- Depending on the type of tumor, treatment can range from various combinations of surgical resection, chemotherapy, radiation and/or immunotherapy.
- Minority groups are traditionally under-represented in clinical trials, and often have difficulty accessing quality care for their child’s tumor.
Pediatric Brain Tumor Notes
Patient History
- Key history components include: location of pain, characteristics, onset, timing, duration, alleviating and aggravating factors, and associated symptoms (e.g., focal weakness, dizziness, loss of consciousness, increased falls, vomiting that alleviates pain, waking from sleep, phono/photophobia).
- In younger kids who may have more difficulty verbalizing their symptoms, parents may notice things like not eating as well, increased vomiting, poor growth/development, fussiness or increased clumsiness (i.e., running into walls).
- Expert Opinion: Oftentimes, a parent will have concern that something is different than before, though they may be unable to specify or verbalize what exactly is different. Dr. Hummel recommends taking this “parent’s intuition” into account.
- Other important history questions include: family history of migraines or headaches (strong predictor of benign headaches), a thorough medication reconciliation (e.g., contraceptive pill or acne medications, which could make other benign differential diagnoses such as idiopathic intracranial hypertension more likely), and a thorough social history (e.g., smoking, caffeine, alcohol or other drug use, stress, trauma).
Physical Exam
Start here.