In addition to the resource below, please see and review Chronic Dyspnea: Diagnosis and Evaluation [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. NITIN BUDHWAR, MD, AND ZUBAIR SYED, MD. Am Fam Physician. 2020;101(9):542-548.
I have excerpted from the above resource after the excerpts from The Curbsiders notes.
I’ve included the summary charts which are excellent but I recommend also reading the complete article.
_____________________________________________________________
The differential diagnosis of COPD [Dyspnea] is from The Curbsiders‘#356 Chronic Obstructive Pulmonary Disease (COPD) Update with Dr. Antonio Anzueto*.
*Gorth D, Askin CA, Witt L, Anzueto A, Williams PN, Watto MF. “#356 Chronic Obstructive Pulmonary Disease (COPD) Update with Dr. Antonio Anzueto”. The Curbsiders Internal Medicine Podcast. https://thecurbsiders.com/episode-list 26 September, 2022.
I have added links to resources on the list.
Differential Diagnosis of COPD [Dyspnea] from the above resource:
- Asthma from emedicine.medscape.com
Updated: May 11, 2022
Author: Michael J Morris, MD, FACP, FCCP - Congestive Heart Failure Imaging from emedicine.medscape.com
Updated: Aug 29, 2022
Author: Vibhuti N Singh, MD, MPH, FACC, FSCA - Bronchiectasis from emedicine.medscape.com
- Bronchiectasis
Updated: Sep 15, 2020
Author: Ethan E Emmons, MD - Bronchiectasis Imaging
Updated: Sep 20, 2017
Author: Brenda L Holbert, MD, FACR
- Bronchiectasis
- Vocal Cord Dysfunction
- Vocal Cord Dysfunction: Rapid Evidence Review JOHN MALATY, MD, AND VELYN WU, MD. Am Fam Physician. 2021;104(5):471-475
- How to do Vocal Cord Ultrasound
- Gulf Coast Ultrasound
- 1:51, Aug 10, 2021
- Obliterative bronchiolitis
- Bronchiolitis Obliterans
- [ PMC free article ] [ PubMed ] Krishna R, Anjum F, Oliver TI. Bronchiolitis Obliterans. [Updated 2022 Jun 19]. In: StatPearls [Internet]. Treasure Island (FL): StatePearls Publishing; 2022 Jan-.
- Bronchiolitis Obliterans
Indications for high-resolution computed tomography (HRCT) in the evaluation of dyspnea.
Idiopathic interstitial pneumonias: HRCT chest approach
Last revised by Dr Yuranga Weerakkody on 14 May 2019 from Radiopedia
ACR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF HIGHRESOLUTION COMPUTED TOMOGRAPHY (HRCT) OF THE LUNGS IN ADULTS Revised 2020 (Resolution 33)
______________________________________________________________
Here are excerpts from Chronic Dyspnea: Diagnosis and Evaluation [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. NITIN BUDHWAR, MD, AND ZUBAIR SYED, MD. Am Fam Physician. 2020;101(9):542-548.
I’ve included the summary charts which are excellent but I recommend also reading the complete article.
Abstract
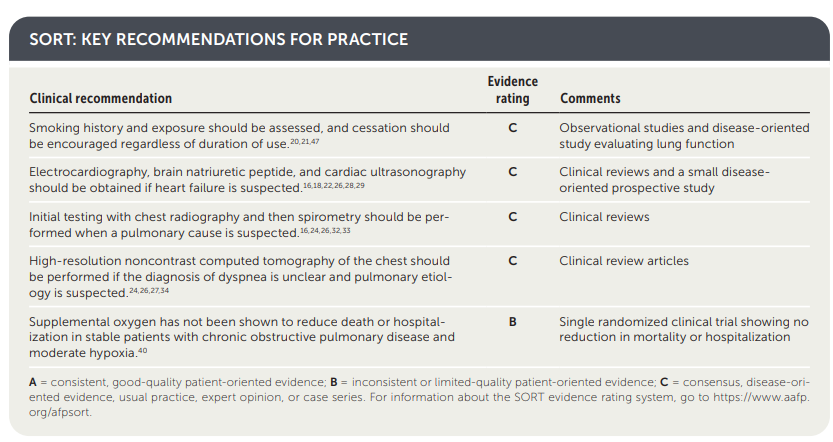
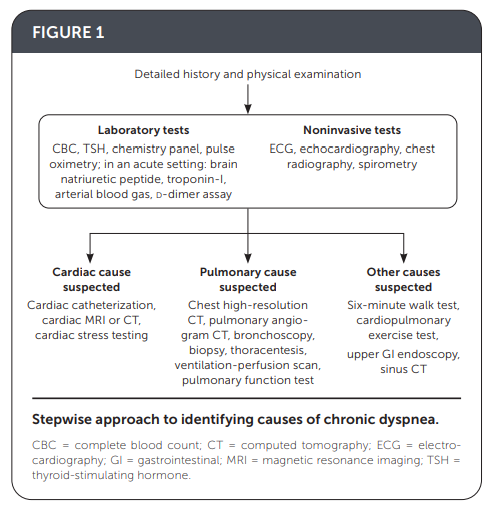
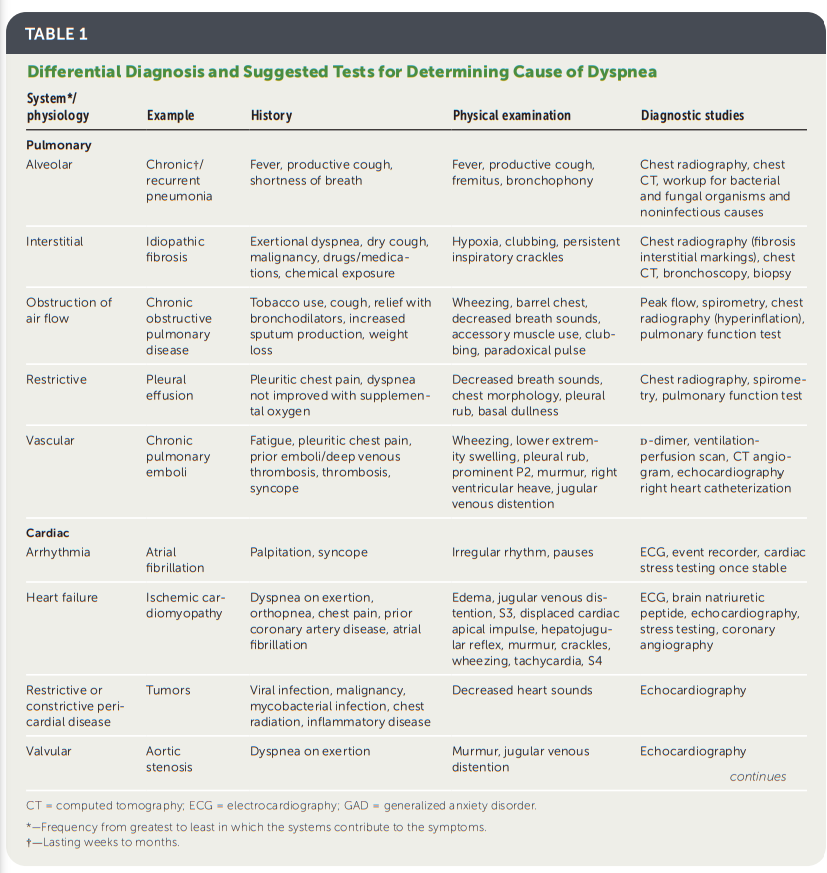
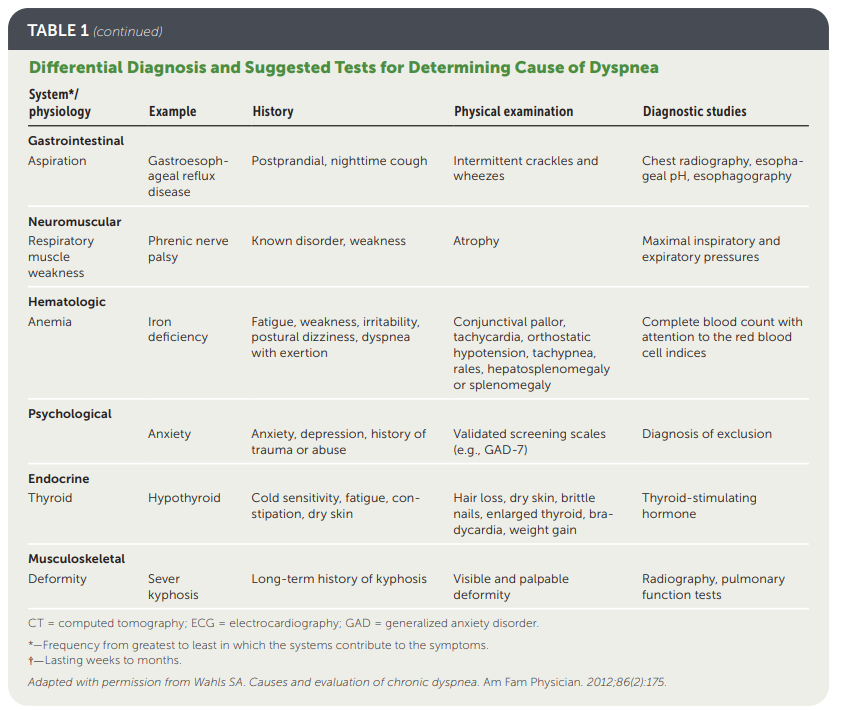
Dyspnea is a symptom arising from a complex interplay of diseases and physiologic states and is commonly encountered in primary care. It is considered chronic if present for more than one month. As a symptom, dyspnea is a predictor for all-cause mortality. The likeliest causes of dyspnea are disease
states involving the cardiac or pulmonary systems such as asthma, chronic obstructive pulmonary disease, heart failure, pneumonia, and coronary artery disease. A detailed history and physical examination should begin the workup; results should drive testing. Approaching testing in stages beginning with
first-line tests, including a complete blood count, basic chemistry panel, electrocardiography, chest radiography, spirometry, and pulse oximetry, is recommended.If no cause is identified, second-line noninvasive testing such as echocardiography, cardiac stress tests, pulmonary function tests, and computed tomography scan of the lungs is suggested.
Final options include more invasive tests that should be done in collaboration with specialty help.
There are three main treatment and management goals: correctly identify the underlying disease process and treat appropriately, optimize recovery, and improve the dyspnea symptoms. The six-minute walk test can be helpful in measuring the effect of ongoing intervention. Care of patients with chronic dyspnea typically requires a multidisciplinary approach, which makes the primary care physician ideal for management. (Am Fam Physician. 2020; 101(9):542-548. Copyright © 2020 American Academy of Family Physicians.)