This blog consists of my study notes. This post contains a link to an excellent resource on digoxin poisoning.
Here is the link to Episode 90 – Low and Slow Poisoning from Emergency Medicine Cases. The episode featured a detailed discussion of the diagnosis and management of both acute and chronic digoxin toxicity. The discussion starts at 50:30 and ends at 1:19:20.
The topic is well covered in the excellent show notes and the key is to go to the show notes and review all the notes on digoxin poisoning. Although the notes are incredibly complete [note to myself], before or after rereviewing the show notes be sure and relisten to this portion of the podcast.
So what follows are the show notes from the podcast relevant to dig toxicity:
On this EM Cases podcast the Medical Director of The Ontario Poison Control Centre and Emergency Physician at St. Michael’s Hospital, Dr. Margaret Thompson, along with Dr. Emily Austin, Emergency Physician and Toxicologist at St. Michael’s Hospital, help us to recognize these overdoses early and manage them appropriately.
Digoxin Poisoning
Chronic digoxin poisoning has a higher mortality, more vague symptomatology, and more low and slow compared to acute digoxin poisoning. Ventricular dysrhythmias are more classically associated with acute digoxin poisoning, though can be seen in chronically poisoned patients as well.
The classic patient with digoxin toxicity is the older patient on their usual dose of digoxin who develops vague symptoms such as ‘weak and dizzy’, altered LOA, nausea and visual symptoms along with low and slow vitals.
Classic triggers for digoxin toxicity in the patient taking their usual daily dose:
- Volume depletion (digoxin is excreted renally)
- Recent medication change (there are many drug-drug interactions with digoxin)
The ECG and Digoxin
First, one must distinguish between digoxin effect and digoxin toxicity.
Digoxin effect: ECG characteristics normally seen in a non-toxic patient taking therapeutic doses of digoxin, displays scooped ST segments, otherwise known as ‘The Salvador Dali Moustache’ after the great surrealist painter.
Digoxin toxicity can cause almost any dysrhythmia except rapid atrial fibrillation. As acute digoxin toxicity often causes hyperkalemia, ECG findings may reflect those of hyperkalemia. (Go to Episode 86 Emergency Management of Hyperkalemia for ECG examples)
Classic digoxin toxicity ECG findings are a result of myocardial irritability or blockade at the AV node and include:
Myocardial irritability:
- Slow atrial fibrillation
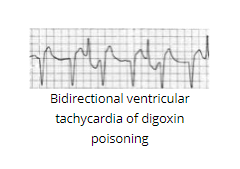
- Bidirectional ventricular tachycardia
- Frequent PVCs
AV blockade:
- Junctional rhythm
- AV dissociation
- Heart block
Pitfalls in Interpreting Digoxin Levels
False positives
- Digoxin levels will always be falsely elevated if taken within 6 hours of ingestion, so you must wait >6 hours to draw the first digoxin level.
- After DigiFab is given, digoxin levels will always be falsely elevated
False negatives
Chronic digoxin toxicity can present with digoxin levels in the therapeutic range, and acute ingestion of nondigoxin cardiac glycosides (e.g. foxglove or oleander)
Treatment of the low and slow digoxin poisoned patient
- Fluid bolus
- Trial of atropine 0.5mg IV
- DigiFab
There is little role for pacing in the slow and low digoxin toxic patient because of increased myocardial irritability and the risk of deterioration into a malignant dysrhythmia.
Transcutaneous pacing may be considered in the unstable slow and low digoxin toxic patient if there is a delay to administration of DigiFab when atropine has failed.
For acute digoxin poisoning with ventricular dysrhythmias, consider IV lidocaine and/or IV esmolol.
Indications for DigiFab antidote
The indications for DigiFab include the following in the setting of suspected digoxin poisoning:
- Hyperkalemia (K >5)
- History of 10mg digoxin ingestion in an adult or 4mg in a child
- Renal Failure
- Ventricular or unstable atrial dysrhythmias
- High digoxin serum level
- Multiple drug ingestions
Dosing DigiFab – a new regimen
In cardiac arrest due to digoxin poisoning give 10 vials of DigiFab and repeat in 15 mins prn x 1 for a total of 20 vials
In chronic digoxin poisoning give 1 vial and repeat prn based on clinical condition, ECG and serum potassium (usually requires approximately 5 vials total)
In acute digoxin poisoning give 2 vials and repeat prn based on clinical condition, ECG and serum potassium (usually requires approximately 10 vials total)
Is calcium safe in hyperkalemic digoxin toxic patients?
Chronic digoxin toxicity typically causes hypokalemia. If a chronic digoxin toxic patient is hyperkalemic it is likely due to acute renal failure and those patients giving calcium is likely safe (unlikely to cause ‘stone heart’).
Acute digoxin toxicity typically causes hyperkalemia due to blockage of Na-K ATPase. These patients do not need anything to stabilize their cardiac membranes or shift potassium. These patients need DigiFab.
When is Intralipipid indicated in digoxin toxicity and how do we administer it?
See my post Lipid Emulsion Therapy – Help From Emergency Medicine Cases Episode 90
Posted on March 15, 2019 by Tom Wade MD.