In this post I excerpt “LAST, prevention, recognition, Rx” from EM Quick Hits 26 LAST, Sodium Nitrite Poisoning, Post-intubation Care, Tetracaine for Corneal Abrasion, ST Segment in Occlusion MI, Coping with COVID. [Link is to the podcast and show notes.] Published February 2021. This segment of the podcast is from 0:54 to 10:51.
Here is the excerpt:
LAST prevention, recognition and management
- LAST (Local Anesthetic Systemic Toxicity) is an iatrogenic life-threatening acute neurologic/cardiac adverse reaction resulting from infiltration of local anesthetic that enters the systemic circulation
- The best treatment is prevention! Preventative measures include aspirating before injection of anesthetic to ensure that the needle is not in a blood vessel and using less than the toxic dose of the anesthetic (see table below)
- Consider LAST in any patient coming from outpatient surgical center in cardiac arrest
- Initial symptoms/signs include perioral numbness and other paresthesias, tinnitus, muscle fasciculations, hypertension, tachycardia progressing to tonic-clonic seizures, decreased LOA, apnea, hypotension, bradycardia, dysrhythmias and cardiac arrest
- Neurologic symptoms typically precede cardiovascular symptoms in lidocaine toxicity while cardiovascular symptoms typically present first in bupivacaine toxicity
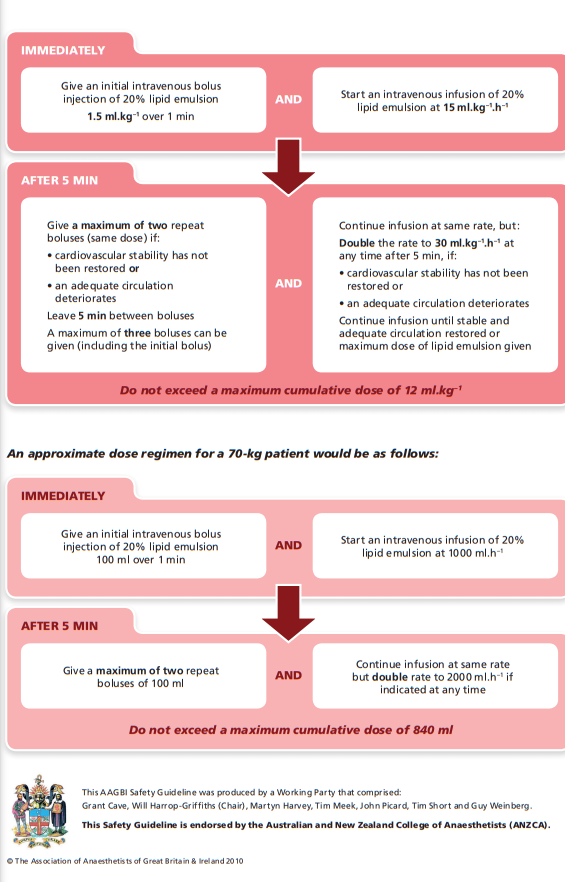
- Treatment in addition to withdrawal of anesthetic and usual CABs may include epinephrine, bicarb, lipid emulsion therapy
References:
- Schwartz DR, Kaufman B. Local Anesthetics. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e New York, NY: McGraw-Hill; 2015.
- Neal JM et al, American Society of Regional Anesthesia and Pain Medicine. American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med 2012;37:16–8.
- Cao D et al. Intravenous lipid emulsion in the emergency department: a systematic review. J Emerg Med 2015; 48(3): 387-97.
Finally, Dr. Helman reviews the points of the above lecture and refers us to Emergency Medicine Cases Episode 90 Low And Slow Poisoning, January, 2017 for much more on the topic. Here is the Introduction:
One of the things we need to think about whenever we see a patient who’s going low and slow with hypotension and bradycardia is an overdose. B-blockers, calcium channel blockers (CCB) and digoxin are some of the most frequently prescribed cardiovascular drugs. And inevitably we’re going to be faced with both intentional and unintentional overdoses from these drugs in the ED. On this EM Cases podcast the Medical Director of The Ontario Poison Control Centre and Emergency Physician at St. Michael’s Hospital, Dr. Margaret Thompson, along with Dr. Emily Austin, Emergency Physician and Toxicologist at St. Michael’s Hospital, help us to recognize these overdoses early and manage them appropriately.
See also Sodium Channel Blocker Toxicity, from StatPearls, Last Update: August 14, 2020. This excellent resource has details on the use of the therapy of sodium bicarbonate and of intralipid.
For a great brief introduction and review of the subject, see Local Anesthetic Systemic Toxicity and Lipid Emulsion Therapy BY DR SEAN M. FOX of Pediatric EM Morsels· PUBLISHED SEPTEMBER 21, 2018.
See also Local Anesthetic Systemic Toxicity (LAST): A Problem-Based Learning Discussion, Feb. 21, 2021 from the American Society of Regional Anesthesia and Pain Medicine.
Please review Management of severe local anaesthetic toxicity below from the Association of Anaesthetists: