In this post, I link to and excerpt from the CoreIM Mind The Gaps podcast, Hyperkalemia in CKD, Posted: November 17, 2021
By: Dr. Larissa Kruger-Gomes, Dr. Shreya P. Trivedi, Dr. Shivam Joshi and Dr. Jeff William
Graphic: Dr. Cathy Cichon
Audio: Daksh Bhatia
All that follows is from the show notes and/or transcript.
Show Notes
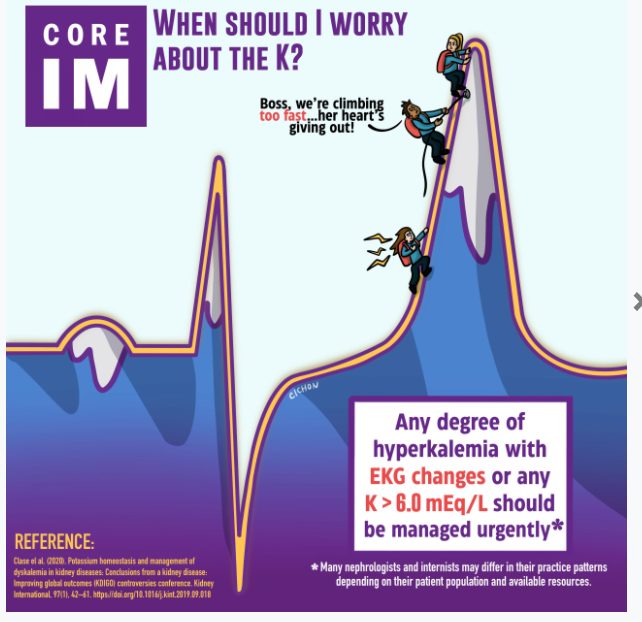
1. Referral for urgent management of hyperkalemia
- Current guidelines from kidney international suggest that the following outpatients should be referred for urgent management:
- K+ > 6.0 mEq/L with OR without ECG changes
- Anyone with hyperkalemia and documented EKG changes
- However, there is no consensus on these recommendations and many clinicians manage hyperkalemia in the outpatient setting differently (especially with hyperkalemia < 6.0 mEq/L)
2. Hyperkalemia and ECG changes
- A retrospective chart review of 90 patients admitted with severe hyperkalemia (K+ > 6 mEq/L) showed only 52% met criteria of having any ECG changes.
- The study authors concluded that the ECG was insensitive for diagnosing hyperkalemia
- Recent retrospective study from 2019 compared ECG findings of 3 groups and found no significant difference in the frequency of ECG changes between the normokalemia (K+ < 5.1 mEq/L) and moderate hyperkalemia (K+ between 6 and 7 mEq/L) groups.
- For every patient including those in the severe hyperkalemia group (K+ > 7.0 mEq/L) more than half did NOT have any ECG changes.
- Take-home point: ECGs are not sensitive in the detection of hyperkalemia. The absence OR presence of EKG changes does not predict the presence of hyperkalemia.
- A Case report from Japan discusses a patient with an initial potassium of 8.5 mEq/L and a normal ECG. It was not until after the patient’s potassium was corrected and then their hyperkalemia acutely recurred that they developed a sine wave pattern on ECG.
- There is no consensus or solid data on what “chronic” hyperkalemia means, with respect to how high or how long a patient needs to have it.
- Take-home point: The abrupt change from normokalemia to severe hyperkalemia, not necessarily the K+ level itself, is most worrisome and needs to be treated.
3. Pseudo-hyperkalemia
- Conditions that lead to pseudo-hyperkalemia, the in vitro release of intracellular K+
- Excessive tourniquet use
- Fist clenching
- Vein trauma from multiple phlebotomy attempts
- PICC/central line draws
- Use of serum separator tube (clot activators) – commonly used to measure the “basic metabolic panel”
- Sending a whole blood sample, sent to the lab in an anticoagulated tube, is the most reliable way to get an accurate potassium reading
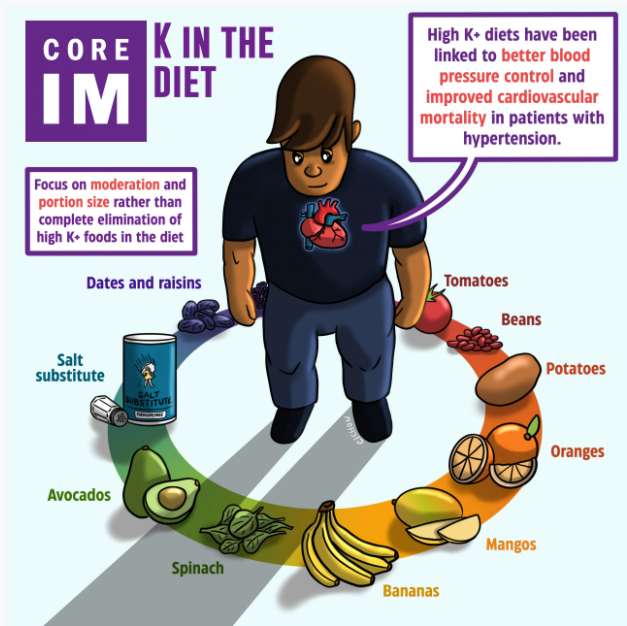
4. K+ restricted diets
- Lots of foods high in potassium are part of a healthy diet such as fruits like; oranges, mangoes, avocadoes, melon, prunes, raisins, and dates.
- Avoid generalization like, “restrict all plant based foods”.
- Some studies suggest that potassium from plant foods (perhaps due to their cell walls) have limited bioavailability and therefore, are poorly absorbed.
- Plant based foods, although potassium rich, have high amounts of fiber and alkali, which can counteract the metabolic acidosis of CKD.
- High potassium diets have been linked to better blood pressure control and improved cardiovascular mortality in patients with hypertension.
- Low potassium diets have been shown to increase sodium reabsorption, and worsen blood pressure control, and can even lead to progression of CKD.
- Pro-tips to avoid Nutritional Confusion:
- Individualize dietary counseling, take a detailed dietary history.
- Salt substitutes are often Potassium Chloride (KCl), and should be avoided.
- Juices and sauces can be high in potassium and do not have significant dietary benefits.
- Constipation and fasting can lead to elevated potassium levels.
- For potato lovers, leaching your potatoes is a great way to reduce their potassium levels.
- Take-home point: Complete elimination of K+ from the diet is not advisable. High K+ foods should be consumed in moderation, as they provide significant cardiovascular health benefits, especially for those with CKD.
5. Key medications that can cause hyperkalemia
- Renin-Angiotensin-Aldosterone System Inhibitors
- RAAS inhibitors improve mortality, but are often the first medications to be discontinued when hyperkalemia is detected.
- It is difficult to predict how much the potassium will improve with stopping a RAAS inhibitor.
- Consider the factors that determine each individual patient’s potassium balance, for example diabetics have lower levels of insulin (or higher resistance) meaning less insulin surge post meal and less intracellular potassium shift.
- Also some patients with diabetes are in a hyporenin hypoaldosteronism state, making the kidney much less efficient at excreting potassium. Use of a RAAS inhibitor in these patients is a recipe for hyperkalemia.
- NSAIDS
- NSAIDs (and beta blockers) decrease renin release (and less RAAS activation), which decreases potassium excretion leading to hyperkalemia.
- Trimethoprim Sulfamethoxazole
- Antibiotics like TMP-SMX block potassium excretion in the collecting duct of the nephron leading to hyperkalemia.
6. Treating outpatient hyperkalemia
- Sodium polystyrene sulfonate (SPS, a.k.a Kayexalate)
- Most of the data on SPS is retrospective, without any RCTs.
- Retrospective cohort study of 1.8 million patients over age 66 showed SPS users had 2x higher rates vs. controls of having GI events like: intestinal ischemia, thrombosis, ulceration, perforation, resection, or ostomy creation.
- Most patients find SPS difficult to drink, as it tastes disgusting inhibiting long term use.
- Patiromer
- Sodium zirconium cyclosilicate, SZC
- Influential trials include HARMONIZE and ENERGIZE.
- The NEJM study in 2015 showed that 1 dose of SZC has a rapid onset, with normokalemia achieved in an average time of 2.2 hours
- Main side effect = occasional edema (from the sodium load), without any increase in blood pressure
- Patient tolerability is much better – easy to take and tasteless