Noninvasive ventilation is also called noninvasive positive pressure ventilation (NIPPV).
Historically, noninvasive negative pressure ventilation was used in the polio epidemic (the iron lung) but noninvasive ventilation currently refers to NIPPV.
This post is about Initial Settings And Titration of Noninvasive Ventilation and is excerpted from Noninvasive Ventilation Sections from emedicine.medscape.com.
What follows are excerpts from the Application of Noninvasive Ventilation webpage [the entire page should be reviewed]:
Proper fitting of the mask or other interface is another key component to successful noninvasive ventilation. The mask or interface may be held in place (without straps applied) by the patient or therapist to familiarize the patient with the mask and ventilator. Typically, the smallest mask providing a proper fit is the most effective. Straps hold the mask in place, with care to minimize excess pressure on the face or nose. Leaks are the bane of all of the interfaces, but excess pressure applied with the straps increases the risk of pressure necrosis and skin breakdown. Straps should be tight enough to prevent leaks, but with enough slack to allow passage of one or two fingers between the face and the straps.
Modes of ventilation
Choosing the initial mode of ventilation is based in part on past experience, in part on the capability of ventilators available to provide support, and in part on the condition being treated. Most patients who are provided noninvasive ventilation are provided support with pressure ventilation, with continuous positive airway pressure (CPAP), which is the most basic level of support. CPAP may be especially useful in patients with congestive heart failure or obstructive sleep apnea.
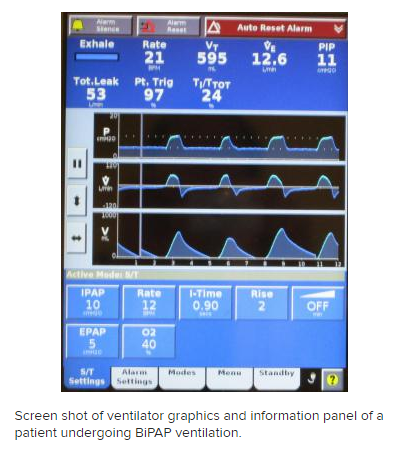
Bilevel positive airway pressure (BiPAP) is probably the most common mode noninvasive positive pressure ventilation and requires provisions for inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). The difference between IPAP and EPAP is a reflection of the amount of pressure support ventilation provided to the patient, and EPAP is synonymous with positive end-expiratory pressure (PEEP). Some noninvasive ventilation is provided using proportional-assist ventilation (PAV), which provides flow and volume assistance with each breath. Clinical trials have not demonstrated a significant difference between PAV and pressure-support ventilation with BiPAP. [5, 6] However, BiPAP is the most commonly available and more frequently used modality for noninvasive ventilation. PAV remains available on many ventilator models, but use is much less common than BiPAP.
Initial ventilator settings and adjustments
Adequate ventilation and oxygenation, correction of respiratory failure, and adequate patient tolerance and comfort are the primary goals of noninvasive ventilation, and adjustments are made to achieve these endpoints. Initial settings focus on achieving adequate tidal volumes, usually in the range of 5-7 mL/kg. Additional support is provided to reduce the respiratory rate to less than 25 breaths/minute. Oxygen is adjusted to achieve adequate oxygenation, with a pulse oximetry goal of greater than 90%. Serial arterial blood gas measurements are essential to monitor the response to therapy and to guide further adjustments in the ventilator. The following provides some guidance on titration of ventilator settings in patients with respiratory distress and who have never been placed on noninvasive ventilation. In those patient who may have chronic noninvasive support, the initial values should be based on prior support levels. The listed levels may be inadequate and would thus increase the likelihood of intolerance or failure. If there is uncertainty, it is important to perform a bedside titration with increasing levels based on patient comfort or exhaled tidal volumes. These adjustments can be made within minutes and can be done without obtaining blood gases.
Initial IPAP/EPAP settings are as follows:
Subsequent adjustments based on arterial blood gas values are as follows:
Pressure control (PC) and average volume assured pressure support (AVAPS) ventilation
The above considerations and approach to adjustment are best suited for those with COPD or chronic heart failure as the primary cause of their hypercapnia or hypoxemic respiratory distress and failure. Patients with neuromuscular disorders (amyotrophic lateral sclerosis, postpolio syndrome, muscular dystrophy) or thoracic cage disorders (severe kyphoscoliosis) may fare better with other ventilatory modalities. [Visit the web page for this complete section.]
AVAPS (average volume assured pressure support*) is another option in these neuromuscular disease patients and has also been used in those with severe obesity-hypoventilation syndrome.
*See Noninvasive mechanical ventilation with average volume assured pressure support (AVAPS) in patients with chronic obstructive pulmonary disease and hypercapnic encephalopathy. [PubMed Abstract] [Full Text HTML] [Full Text PDF] From the Abstract Background: Non-invasive mechanical ventilation (NIV) in patients with acute respiratory failure has been traditionally determined based on clinical assessment and changes in blood gases, with NIV support pressures manually adjusted by an operator. Bilevel positive airway pressure-spontaneous/timed (BiPAP S/T) with average volume assured pressure support (AVAPS) uses a fixed tidal volume that automatically adjusts to a patient’s needs.
Resuming excerpts from the web page Application of Noninvasive Ventilation:
As with any pressure-cycled mode [for example Bi-PAP], the dependent variable is volume and it may vary widely if there is patient dyssynchrony, changes in lung compliance, or changes in resistance that can occur with changes in body position that occurs in the very morbidly obese. A fixed pressure support setting will not compensate for these changes, and, as a result, delivered tidal volume will fall. AVAPS allows a target tidal volume to be identified with a range of pressure support settings that fluctuate to meet the target tidal volume. AVAPS uses an internal algorithm to make changes in the pressure support supplied to achieve the target volume, but these changes are small and occur over minutes (typically 1-2.5 cm water per minute). That is why rapidly changing, acute respiratory conditions are not suited for AVAPS as the ventilator adjustments may not be timely enough to meet the patient’s requirements. Typically, the pressure support required to produce the target volume during bedside titration is used to identify the minimal pressure with the set minimal pressure (min P), typically 2-3 cm water lower to allow flexibility for adjustment in the AVAPS mode. The maximal pressure (max P) is typically set in the 20-25 cm water range as higher pressures are not well tolerated. The min P is at least 8 cm water and usually higher. Additional parameters that are part of AVAPS setting are the target tidal volume, respiratory rate, EPAP, and inspiratory time.
See also:
- Overview, Indications, And Contraindications for Noninvasive Ventilation From Emedicine.medscape Posted on June 11, 2017 by Tom Wade MD
- Predictors of Success, Failure, And Need For Intubation In Noninvasive Ventilation From Emedicine Posted on June 13, 2017 by Tom Wade MD