Today, I link to, review, and excerpt from Dr. Lichtenstein’s The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure [PubMed Abstract] [Full Text HTML] [Full Text PDF] Critical Ultrasound Journal [Open Access but now called The Ultrasound Journal]. August 2011, Volume 3, Issue 2, pp 109–110.
The above 2010 article covers much of the same material as his 2017 article, Novel approaches to ultrasonography of the lung and pleural space: where are we now? [Link is to the 2017 full text PDF].
Today, I’m reviewing, linking to, and excerpting from the 2010 article because it covers the material very succinctly and is a great summing up of the much more comprehensive 2017 article.
Previously, I linked to, reviewed, and excerpted from the more recent 2017 article [cited above] from Dr. Lichtenstein in two posts:
- Links To And Excerpts From The First Part-The Basics-Of Dr. Lichtenstein’s Article On How To Perform Lung Ultrasound In The Critically Ill With Additional Resources. Posted on December 1, 2019 by Tom Wade MD
- Links To And Excerpts From The Second Part-The Basics-Of Dr. Lichtenstein’s Article On How To Perform Lung Ultrasound In The Critically Ill With Additional Resources. Posted on December 1, 2019 by Tom Wade MD
First, I quote Dr. Lichtenstein’s 7 principles of lung ultrasound in the critically ill (LUCI) from his 2017 article:
The seven principles of LUCI
The seven principles of LUCI have not changed since
2001 [6], apart from a slight update to principle 7
- A simple technique is still suitable.
- The thorax is an area where air and water (gas and fluids for purists) can mingle. They follow the rules of gravity. One can define a macro-gas/fluid ratio (e.g. pleural effusion and aerated lung) and a micro-gas/fluid ratio, for defining the situation where in a minute place, the two elements coexist (e.g. an oedematous subpleural interlobular septum surrounded by air).
- The lung is the widest organ; areas of interest must be defined (the BLUE points).
- All signatures arise from the pleural line.
- Artefacts, although usually considered a hindrance, have critical relevance in lung ultrasound.
- The lung is the most vital organ. Like all vital organs, it is dynamic. The main dynamic is referred to as lung sliding.
- All life-threatening disorders abut the chest wall, [Update: and almost all, even small ones,] have an extensive location (e.g. a pneumothorax can be small but visible in a rather large projection).
Here are excerpts from Dr. Lichtenstein’s 2010 article The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure [Links above]:
Studies have shown that most acute lung disorders benefit from [examining the lung in] standardized locations.
Clinically relevant interstitial syndrome locates anteriorly [4].
Free pneumothoraces always locate anteriorly [5].
As free fluidsfollow gravity rules [6], all cases of free pleural fluid effusion, regardless its abundance locate at least posteriorly above the diaphragm [7].
Lung consolidation can locate everywhere depending on the cause and extension, yielding sensitivity lower than other disorders, 90% [8], yet its posterior location above the diaphragm in critically ill patients with pneumonia is usual [4].
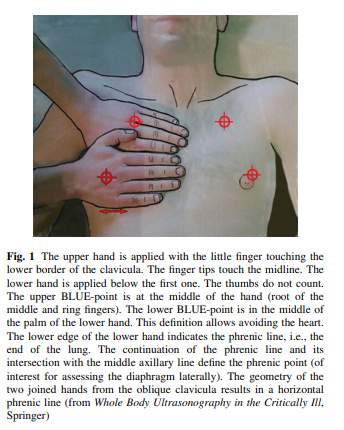
We consider the hands of the patient (called BLUE hands, roughly standard doctor’s hands size in standard adults; physicians with large or small hands would make the adaptation once for all). The hands, applied as shown in
Fig. 1, define the anterior chest wall.This is of great help in patients with major obesity, nipple ptosis, etc.
This works with patients of any size, neonate included [It is the size of the patient’s hands that is used-i.e. two hands of the size of the neonate are applied to the anterior chest].
The BLUE-hands allows to define five regions of interest. The
upper and lower BLUE-points, the phrenic line, defined in
Fig. 1, are anterior.
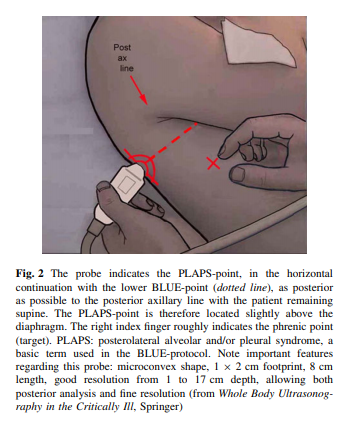
The phrenic point is lateral, defined in Fig. 2. The PLAPS-point, defined in Fig. 2 from the lower BLUE-point, is posterior.
The PLAPS-point, defined in Fig. 2 from the lower BLUE-point, is posterior.
The upper BLUE-point immediately informs on pneumothorax (A’-profile) in semirecumbent (i.e., Stage 1′, usually performed in dyspneic, nonventilated) patients.
The lower BLUE-point immediately informs on pneumothorax
in supine (i.e., stage 1, performed on mechanical ventilation) patients.The upper and lower BLUE-points immediately inform on pulmonary edema (B-profile) or immediately suggest pulmonary embolism (A-profile).
The PLAPS-point allows immediate diagnosis of pneumonia,
when combined with negative anterior findings among others [4].Note that the BLUE-points are not appropriate for subtle approach of ARDS, nor for comprehensive search of small anterior (C-profile) or lateral consolidations, requiring more liberal scanning.
The lung point, as opposed to the BLUE-points, is located according to the pneumothorax extent [9]*.
* Please see Links To And Excerpts From “Sonographic diagnosis of pneumothorax.”
Posted on December 5, 2019 by Tom Wade MD.
Returning now to Dr. Lichtenstein’s 2010 article:
In the BLUE-protocol, we advise a 5-MHz microconvex
probe resulting in a small footprint, and a good resolution
for both superficial and deep disorders (Fig. 2). This probe
also allows satisfactory analysis of the vessels, heart, optic
nerves, belly, i.e., whole body analysis, neonate excepted
[2].Those who do not benefit from [the above] probe will need the
good resolution of abdominal probes for the anterior
analysis of the artifacts, the good superficial resolution of
linear probes for details on lung sliding, and the good
ergonomy of cardiac probes for PLAPS detection, taking
maximal care for disinfecting each probe between changes,
which prevents the BLUE-protocol to be performed within
3 min as advocated [4].