In this post I link to and excerpt from ECG Cases 18 – ST Depressed Mnemonic And Occlusion MI from Emergency Medicine Cases, by Dr. Jesse McClaren, February 8, 2021.
Note to myself when reviewing: First review the notes below from Dr. McClaren’s post and then go to the post itself to test myself by reviewing the ten ECGs he has provided for us.
All that follows is from Dr. McClaren’s post:
In this ECG Cases blog we look at 10 patients who presented with potentially ischemic symptoms and ST depression. Which had occlusion MI?
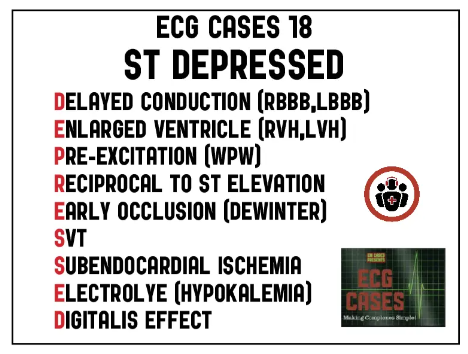
ST ‘DEPRESSED’ mnemonic and occlusion MI
As a review of ST depression explained, “In many instances, STD is associated with acute coronary syndromes (ACS)—both acute ischaemia and acute infarction; this electrocardiographic pattern, however, may also be found in patients with non-ischaemic events, such as left bundle branch block (LBBB), left ventricular hypertrophy (LVH), and those with therapeutic digitalis levels. Proper interpretation of the ECG in these patients will assist the clinician in arriving at the correct diagnosis—in effect, separating acute coronary syndrome from the non-ischaemic, more ‘benign’ causes of STD”[1]
Step 1: Differentiate ST depression that is secondary to abnormal conduction (bundle branch block, ventricular hypertrophy, or pre-excitation) from primary ST depression.
Step 2: Determine the cause within these two broad categories. This approach, and differential, is summarized by the mnemonic ‘DEPRESSED’:
Secondary to abnormal conduction
- Delayed conduction (RBBB, LBBB/paced)
- Enlarged ventricle (LVH, RVH)
- Pre-excitation (WPW)
Primary: acute coronary occlusion
- Reciprocal to ST elevation
- Early occlusion (deWinter T wave)
Primary: supply/demand mismatch
- SVT (rate related)
- Subendocardial ischemia (including non-occlusive MI, massive GI bleed, PE, sepsis)
Primary: metabolic/medication
- Electrolye (hypokalemia)
- Digitalis
Like the differential for ST elevation, there can be baseline secondary ST depression with superimposed primary changes—which disproportionate ST changes can help identify (eg modified Sgarbossa criteria for LBBB, or concordant/disproportionate ST changes in RBBB). While the STEMI paradigm dichotomizes ST elevation and ST depression, early occlusion can manifest as ST depression only (eg. DeWinter T waves with ST depression and hyperacute T waves), and both ST elevation and depression can co-exist in the same ECG and represent the same current of injury. As a couple of cardiologists explained a decade ago, “the STEMI and non‐STEMI differentiation ignores one of the basic tenets of electrocardiography, that is, that any deflection will produce a reciprocal image 180 degrees removed, on the opposite aspect of the field. (Contemplation of V1 and V6 in the setting of bundle branch block or of ventricular hypertrophy should make this concept abundantly clear.) In simple terms, during myocardial infarction, ST elevation or depression are in fact identical entities, that is, a result of an injury current viewed from opposite aspects of the electric field of the heart.”[2]
In some cases of occlusion MI (OMI) the reciprocal ST depression is more obvious than the ST elevation. In inferior OMI, ST depression in aVL can highlight subtle inferior ST elevation and/or hyperacute T waves. In posterior OMI, reciprocal ST depression isolated to the anterior leads can be more obvious than the small degree of ST elevation on the posterior leads. On the other hand, ST elevation in aVR is not “STEMI-equivalent” but is reciprocal to diffuse ST depression—with a broad differential including baseline LVH, subendocardial ischemia (from non-occlusive MI, PE, sepsis or GI bleed) or OMI.
So the real question is not whether it’s a “STEMI” or “NonSTEMI” but what is the cause of the ST changes, and whether it reflects OMI (i.e. total or near-total occlusion with insufficient collaterals, leading to rapid myocardial necrosis) or a non-occlusive MI (NOMI). As a new study found, only 60% of OMIs met STEMI criteria, and the 40% of STEMI(-)OMI had delays to reperfusion and adverse outcomes more similar to STEMI(+)OMI than NOMIs[3].
Now go to Dr. McClaren’s post and test yourself against his ten ECGs.
And when you analyze the ECG, use the H E A R T S template to analyze the rhythm.
So, the first time through, I’m going to go thru the H E A R T S template answer for each of the ten ECGs. So go to the post and to the second ten ECGs after Dr. McClaren’s great tachycardia review notes. I’ll list the ten H E A R T S template answers for my review.
Returning to Dr. McClaren’s post:
10 patients presented with potentially ischemic symptoms and ST depression. Which had occlusion MI?
Case 1: 75yo with one day of shortness of breath and diaphoresis. HR 110, BP 120. Old then new ECG
Case 1: LBBB with STEMI(-)OMI(+)
- Heart rate/rhythm: sinus tach
- Electrical conduction: new LBBB
- Axis: normal
- R-wave: delayed R wave progression from LBBB
- Tension: can’t assess LVH
- ST/T changes: concordant STD in V3 (Sgarbossa)* and disproportionately discordant STD in V4 (STD/R wave>0.30, modified Sgarbossa)*
Impression: “new LBBB” is not an indication for cath lab activation, but this ECG was diagnostic of LBBB + OMI, missed by computer and physician until patient had VF arrest. Cath lab activated after ROSC: 95% circumflex occlusion, peak troponin I = 50,ooo ng/L
*Please review Sgarbossa Criteria by Drs. Mike Cardogan and Robert Butner, March 19, 2021 from Life In The Fast Lane.
*And please see STEMI in the Presence of LBBB, accessed 3-26-2021, from Emergency Physicians Monthly. This is an excellent article on the Sgarbossa Criteria.