In this post, I link to and excerpt from the Cribsiders‘ #42 [Pediatric] Inflammatory Bowel Disease-Go With Your Gut. JANUARY 19, 2022 By SAM MASUR
All that follows is from the above resource.
Summary
Scope out our conversation about Crohn’s and Ulcerative Colitis with our guest, Dr. Ghassan Wahbeh, a pediatric gastroenterologist and director of the IBD center at Seattle Children’s Hospital. Hear his take on what to consider when suspecting inflammatory bowel disease, the best tests to tee up the diagnosis quickly, and the ever-expanding treatment options. This episode is sure to make a splash!
IBD Pearls
- The causes of IBD are multifactorial and largely unknown. Patients and their families should be reassured early that they did not do anything to provoke disease.
- If considering between IBD and celiac, testing for celiac markers may be skipped if an [upper GI] endoscopy is imminent, as biopsy is the gold standard for the diagnosis of celiac disease.
- Top-down therapy not only gets children to the right medications faster, but has shown better outcomes overall.
Diarrhea Workup from emedicine.medscape. com
Updated: Jan 31, 2020
Author: Stefano Guandalini, MDIBD Notes
Defining our Terms:
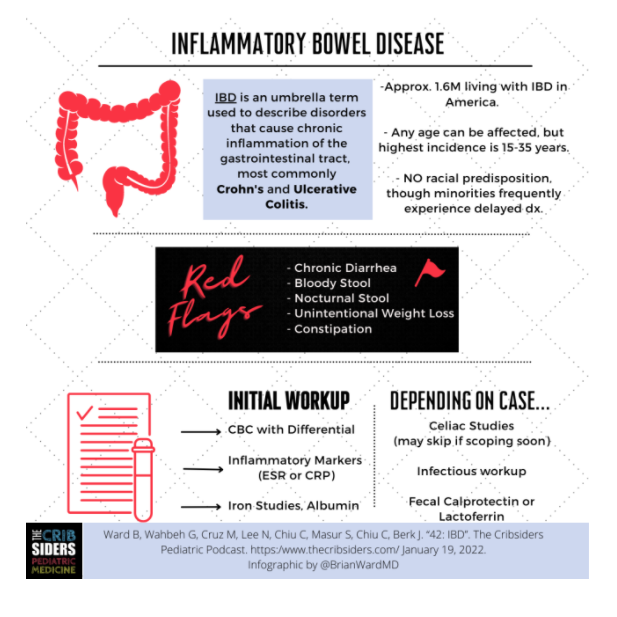
Inflammatory Bowel Disease: an umbrella term used to describe disorders that cause chronic inflammation of the gastrointestinal tract, most often Crohn’s and Ulcerative Colitis(UC). While very similar, Crohn’s and UC differ in a number of ways:
- Crohn’s: Inflammation can be anywhere from mouth to anus and affects all layers of the intestine.
- Ulcerative Colitis: Inflammation is usually confined to the large intestine and only affects the first layer (mucosa) of the large intestine.
IBD includes a large spectrum of overlapping phenotypes. Instead of limiting the diagnosis to either Crohn’s or UC, Dr. Wahbeh likes to describe inflammatory patterns as personal to each patient (expert practice).
The cause of IBD is unknown and likely multifactorial. There is a moderate genetic link, with twin concordance of Crohn’s disease between 35 and 50%. About half of patients with Crohn’s disease have a family member with the same diagnosis. Families should be reassured that they did not do anything wrong to lead to this process.
Incidence is bimodal by age, with peaks at 10-20 yrs old and 20-40 years old, but people of any age can be diagnosed with IBD.
Disparities:
While IBD affects different subgroups of the population (including race and socioeconimic status [SES]) at the same rate, studies have shown a delay in diagnosis for African-American or Black identifying patients, as well as a delay in initiating the most effective treatments for groups of lower income.
An Incomplete Differential Diagnosis for IBD
While the list of differential diagnoses to consider is long, the following are important disease processes that you should consider and/or rule-out when evaluating for IBD.
- Chronic infections
- Immunodeficiencies
- Chronic exposure to Giardia
- Malabsorption
- Celiac disease: roughly 1% of the North American population
- Dietary causes
- Lactose intolerance
Red Flags for IBD
- Chronic diarrhea (2+ weeks)
- Bloody diarrhea
- Kids past 6-7 yrs are generally private about stools or don’t look before they flush.
- Blood in stool comes from ulcerations in the highly vascular lining.
- Presence should raise suspicion, but absence does not rule out IBD.
- A “GI bug” limited to only one person in the family.
- Constipation
- Inflammation in the rectosigmoid colon can act as a barrier, slowing gut transit.
- Unintentional weight loss:
- Infections can cause acute weight loss due to diarrhea or dehydration, but weight loss due to dehydration corrects with rehydration.
- Don’t be fooled by high BMI– unintentional weight loss should not be ignored in patients of any size.
- Waking up at night to use the restroom.
Helpful Initial Tests:
Helpful Initial Tests:
High Value
- CBC with differential
- Inflammatory Markers (ESR, CRP)
- Either ESR or CRP are sufficient.
- ESR usually requires more blood.
- Iron Studies
- Iron Levels.
- Ferritin (note: ferritin is an acute phase reactant).
- Iron Saturation.
Less High Value, but May be Warranted
- Celiac Markers (IgA Tissue Transglutaminase)
- Can consider skipping this if an upper endoscopy is imminent (biopsy is the gold standard for a diagnosis of celiac disease).
- Infectious stool studies
- If chronic exposure to Giardia is suspected, for example
- Stool calprotectin or lactoferrin (which is generally institution specific)
- Calprotectin is a dominant protein in the cytoplasm of neutrophils.
- Will indicate inflammation, but won’t differentiate the cause (infection vs. IBD).
- Can be negative and falsely reassuring in patients with only small bowel inflammation.
Lower Value/Don’t Do!
- Stool Guaiac/Hemoccult
- Very user dependent with a high degree of false positives (including recent ingestion of NSAIDs, red meat, and broccoli. Yes, I said broccoli!).
The Ins and Outs of Endoscopy
Timeline of when to scope should be based on severity of symptoms as well as lab tests. Some children with high levels of anemia, uncontrollable pain, or challenges keeping up with hydration may require admission and next-day scope.
Kashlack Children’s aims for performing endoscopy within 1-2 weeks, but institutional practices may vary.
Waiting for a scope can be a very anxious time for a family. Make sure to reassure them, when appropriate. Though very serious and challenging for patients and families, IBD is rarely life-threatening.
Children (more often than adults) have upper and lower tract inflammation, so usually both upper and lower endoscopy will be done.
Noncaseating granuloma (collection of coalescing macrophages) are the hallmark of Crohn’s.
There can be histologic inflammation in areas that look grossly normal on scope.
Starting medications: Get in the zone, the predni-zone!
Meds will vary based on what is seen on the endoscopy, balancing side effects with the goals of therapy.
Goals of IBD care:
- Improve patient symptoms..
- Normal growth, activity levels, and unimpeded puberty and bone development.
Top-down vs. step-up therapy:
The “traditional” treatment model of step-up therapy has generally given way to top-down therapy for a variety of reasons, including:
- The pediatric IBD phenotype is overwhelmingly moderate-to-severe.
- When doing step-up therapy, about 2/3 of patients require stepping up.
- Treating IBD aggressively early has led to better long-term outcomes. Additionally, aggressive up-front therapy leads to an increased percentage of children experiencing mucosal healing.
Classes of Medication Used
Steroids:
Improve pain, reduce diarrhea, increase appetite, but they do not induce deep mucosal healing as well as other classes of medications. As Dr. Wahbeh says: “it is a great band-aid”
Mesalamine:
A molecule similar to aspirin, this acts as a topical anti-inflammatory. Good for isolated colonic inflammation. The many formulations of mesalamine are based on where the medication will “release” in the gut. There are no head-to-head trials among mesalamines.
Immunomodulators:
Medications like azathioprine and mercaptopurine can be used at moderate doses to decrease immune activity and thereby lessen intestinal inflammation.
Biologics and small molecules:
These newer medications target specific immune cells and cytokines involved in inflammation.
Since their introduction almost 30 years ago, they have been very successful in IBD care. Infliximab and adalimumab were the first biologic medications for pediatric IBD. Since then, many more have been approved, including certolizumab, golimumab, and vedolizumab.
These medications have a diversity of mechanisms including anti-TNF-alpha, anti-IL12/23, anti-adhesion molecules, etc. Small molecules target specific pathways as well.
The biology of inflammation is not static! As patients take these medications, the character of their inflammation may change, resulting in loss of efficacy or in prolonged deep remission. Little is known about this process.
Enteral Nutrition:
Diets of complete enteral nutrition with shakes (usually commercial brand shakes) change the antigenic stimulation within the gut and can improve the symptoms and reduce the inflammation. Inflammation reduction from exclusive enteral nutrition has been shown to be similar or even better than corticosteroids.
Living Life with IBD
The goal of children with IBD is remission—biochemical, symptomatic, and mucosal/endoscopic.
Children in remission can live normal lives with minimal restrictions. The medications can cause immunodeficiencies, but children can live generally unrestricted lives with rare exceptions (Dr. Wahbeh might recommend against spelunking or tuberculosis outreach).
COVID vaccine: not contraindicated. If a patient is on a regularly timed medication like a biologic, try to schedule halfway in-between doses, though this is not an evidence-based recommendation.