Note to myself: I posted on this Curbsiders episode on March 11, 2020 in Polycystic Ovary Syndrome With Katherine Sherif MD From #198 Of The Curbsiders With Additional Resources.
I wanted to review the episode again and hence the repost. This post will be a more complete.
The only reason to check out the earlier post is for the additional resources which I have also included below:
Additional Resources:
(1) Anti-Müllerian hormone (AMH) in the Diagnosis of Menstrual Disturbance Due to Polycystic Ovarian Syndrome [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Front Endocrinol (Lausanne). 2019 Sep 26;10:656. doi: 10.3389/fendo.2019.00656. eCollection 2019.
(2) Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Endocr Soc. 2019 Aug 1; 3(8): 1545–1573.
(3) Recent advances in biochemical and molecular analysis of congenital adrenal hyperplasia due to 21-hydroxylase deficiency [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Ann Pediatr Endocrinol Metab. 2016 Mar;21(1):1-6. doi: 10.6065/apem.2016.21.1.1. Epub 2016 Mar 31.
(4) Diagnosis and Treatment of Polycystic Ovary Syndrome [PubMed Abstract] [Full Text HTML] [Full Text PDF]. AFP, Jul 15, 2016 Issue
In this post I link to and excerpt from The Curbsiders‘ March 9, 2020 podcast and show notes, #198 PCOS: Polycystic Ovary Syndrome with Katherine Sherif MD, by Dr. Molly Hublein.
All that follows is from the above episode:
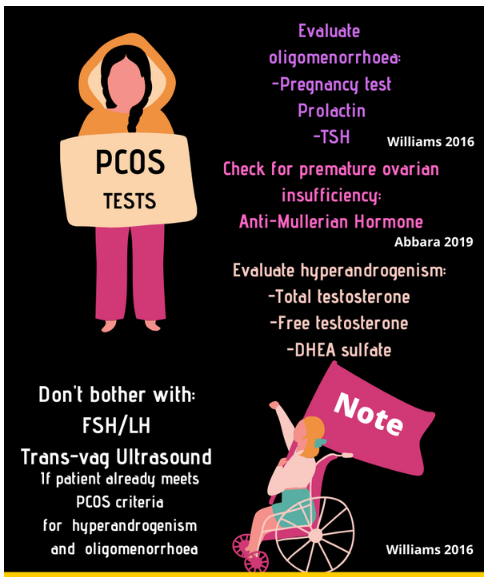
Polycystic ovary syndrome (PCOS) is more common than we think! [10 to 20% of all women, Dr. Sherif states.] Listen as our esteemed guest Dr Katherine Sherif (@katherinesherif) reviews common patient complaints that should trigger PCOS in the differential, its pathophysiology, key physical exam findings, an algorithm for lab evaluation for PCOS diagnosis, and common treatments (OCPs, metformin, spironolactone and more!).
PCOS Pearls
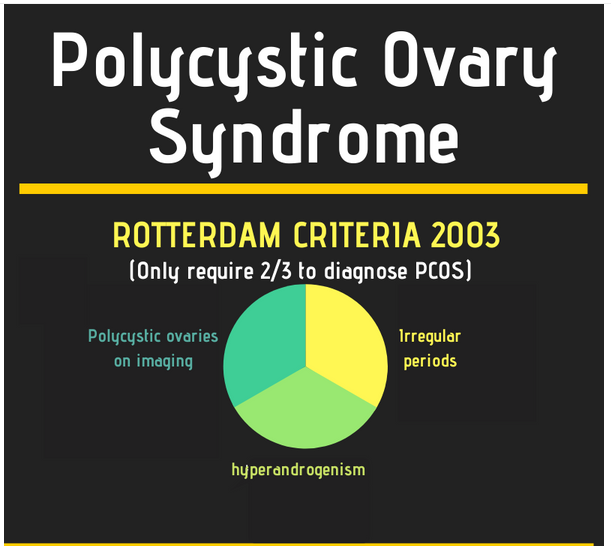
- To diagnose PCOS, patients need any 2 of the following 3: oligomenorrhea, hyperandrogenism, and/or polycystic ovaries seen on imaging
- The underlying cause of PCOS is controversial, but may be related to abnormal hypothalamic-pituitary-ovarian signaling or primary insulin resistance.
- PCOS can manifest with many dermatologic complaints including hirsutism, alopecia, and acne related to hyperandrogenism and acanthosis nigricans, skin tags, and hidradenitis suppurativa related to insulin resistance
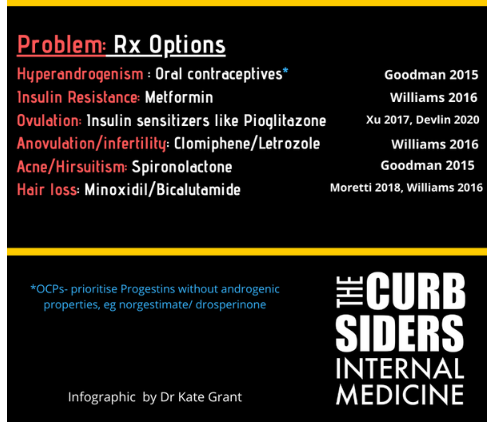
- Treatment for PCOS can include oral contraceptive pills, androgen blockers, and/or insulin sensitizing medications.
Polycystic Ovary Syndrome (PCOS) Defined:
2003 Rotterdam Criteria: to diagnose PCOS a patient needs any 2 of 3: 1. irregular periods (oligomenorrhea/amenorrhea); 2. Signs of hyperandrogenism or laboratory evidence of hyperandrogenism; and/or 3. polycystic ovaries seen on imaging. (Williams 2016)
Patients can have normal ovarian imaging (no polycystic ovaries on ultrasound) or no obesity and still have PCOS if they have irregular periods and hyperandrogenism.
Over 10-20% of women in the US meet criteria for PCOS, this incidence is significantly increasing as we see rises in obesity. (Abbara 2019)
Pathophysiology of PCOS:
We don’t exactly know what drives the development of PCOS. There are several ideas about the underlying pathophysiology. (Witchel 2019)
It may be disordered hypothalamic function drives the pituitary to release excess luteinizing hormone (LH) over follicle stimulating hormone (FSH). High LH will trigger production of more androgens, inhibiting folliculogenesis in the ovary.
Dr Sherif believes the more important driving factor is insulin resistance. Insulin itself directly stimulates the thecal cells in the ovary causing increased androgen production. Insulin goes to hypothalamus increasing pulses of gonadotropin releasing hormone, causing the pituitary to produce more LH, which then impacts ovarian function. Insulin decreases sex hormone binding globulin (SHBG) which releases free testosterone which inhibits folliculogenesis. Insulin resistance contributes to central weight gain, from increased androgens and direct signals to adipocytes.
Common presenting complaints:
Missed/irregular menses, hirsutism, and difficulty losing weight are common presenting complaints that should make you think of PCOS. Most often patients won’t come to PCP for infertility, since they will more likely be directing this complaint to a gynecologist. The irregular menses should be more than 6 weeks apart (oligomenorrhea), not irregular spotting.
Hyperandrogenism:
Hirsutism: Midline terminal hair (darker, coarser) is more related to androgen excess- midline chest hair, midline lower abdominal hair below umbilicus/above pubis, and hair down the inner thighs are signs of hirsutism. Upper arm hair or upper back terminal hair is a strong sign of hyperandrogenism. Hair around nipples or facial hair can be normal and are genetically dependent. (Martin 2018)
Alopecia tends to be the most distressing symptom of PCOS in Dr Sherif’s experience because this is hard to treat and hair is highly socially valued. The hyper-androgen driven alopecia is diffuse– so you see a wider visible scalp part (not patchy like alopecia areata). (Martin 2018)
Severe acne is a sign of hyperandrogenism, especially when it spreads onto upper chest, upper arms, and/or buttocks. Use of isotretinoin treatment in adolescence is significantly correlated with high androgens/PCOS. (Goodman 2015)
Insulin resistance:
Other skin findings including hidradenitis suppurativa, acanthosis nigricans, keratosis pilaris, and skin tags are associated with insulin resistance and PCOS. (Misitzis 2019)
Difficulty with weight loss is common in patients with PCOS, though in Dr Sherif’s experience, about 20% of women with PCOS are lean.