In addition to today’s post, please see Links To And Excerpts From The Curbsiders’ #188 GERD and Dyspepsia with Dr. Amy Oxentenko MD With A Link To The 2021 ACG Guideline For The Diagnosis And Management Of Gastroesophageal Reflux Disease
Posted on March 22, 2022 by Tom Wade MD
In this post, I link to and excerpt from The Curbsiders’ #322 H. Pylori Infection, FEBRUARY 21, 2022 By BETH GARBITELLI.
All that follows is from the above resource.
Take Home Points
- Remember H. pylori is a carcinogen! It is a causative agent in gastric cancer and if found it needs to be treated, with confirmation of eradication.
- Avoid H. pylori serologies for identification of the organism, you want to stick to stool antigen, urea breath test, or endoscopy with biopsy.
- Do not use clarithromycin triple therapy! Choose quadruple therapy.
Tips and tricks for healing up patients with helicobacter!
Say hi and bye to H. pylori infections! We review the basics of H. pylori screening, refresh your memory on testing basics, discuss treatment strategies, and talk through eradication testing with gastroenterologist Dr. George Saffouri (@gbsaff).
A special thanks to our listener Ana Maria Keilhauer Varona (@KeilhauerMa) of @UFMedu who pitched this episode. Her hard work formed the basis for our script!
H.Pylori Pearls
- Dr. Saffouri wants us to not use the term ‘gastritis’ off the bat for a symptomatic diagnosis! Gastritis is a histopathologic diagnosis that requires a biopsy showing inflammatory cell infiltrates (Shah 2021).
- Remember H. pylori is a carcinogen! It is a causative agent in gastric cancer and if found it needs to be treated, with confirmation of eradication.
- Approach screening with a mindset of global and cultural competence. While H. pylori is reported as ‘low prevalence’ in the United States, other global regions have higher prevalence. As such, some guidelines recommend screening in first-generation immigrants from high prevalence countries (El-Serag 2018).
- Avoid H. pylori serologies for identification of the organism; stick with stool antigen, urea breath test, or endoscopy with biopsy.
- Before testing, patients should be off of proton pump inhibitors (Crowe 2019), antibiotics, and probably H2 receptor antagonists for a month (per Dr Saffouri’s practice, the guidelines indicate 1-2 weeks off PPI and 4 weeks off antibiotics, Chey 2017).
- Do not use clarithromycin triple therapy! Given high rates of clarithromycin resistance, choose bismuth-based quadruple therapy.
H. Pylori Show Notes
Classifying Upper GI Symptoms
Helicobacter pylori (h.pylori) infection may present with non-specific abdominal pain, gas, bloating, belching, postprandial fullness, and other symptoms suggestive of dyspepsia(Diaconu 2017).
Dr. Saffouri wants us to not use the term ‘gastritis’ off the bat for a symptomatic diagnosis! Gastritis is a histopathologic diagnosis that requires a biopsy showing inflammatory cell infiltrates (Shah 2021). However, Dr. Saffouri reports it is commonly used as a catch-all diagnosis for patients presenting with epigastric pain.
In terms of the history, Dr. Saffouri recommends asking about red flag symptoms (Crowe 2019) such as bleeding, unintentional weight loss, as well as delving into the type, duration, frequency, and dosing of NSAID usage. Check out our episode on GERD and Dyspepsia with Dr. Amy Oxentenko for more on the work-up of those conditions.
Both GERD and dyspepsia are frequently treated with an initial course of proton pump inhibitors (PPI). However, in dyspepsia it is prudent to evaluate for H. pylori due to the treatable nature of the infection and the long-term gastric cancer risk reduction benefits (Crowe 2019, Chey 2017).
In patients older than 60 y/o, EGD is indicated to evaluate dyspepsia symptoms primarily to assess for malignancy, but also allows for gastric biopsy for evaluation of H. pylori infection. Below 60 y/o, evaluate for H. pylori via urea breath and stool antigen testing (Crowe 2019, Chey 2017).
Screening Basics
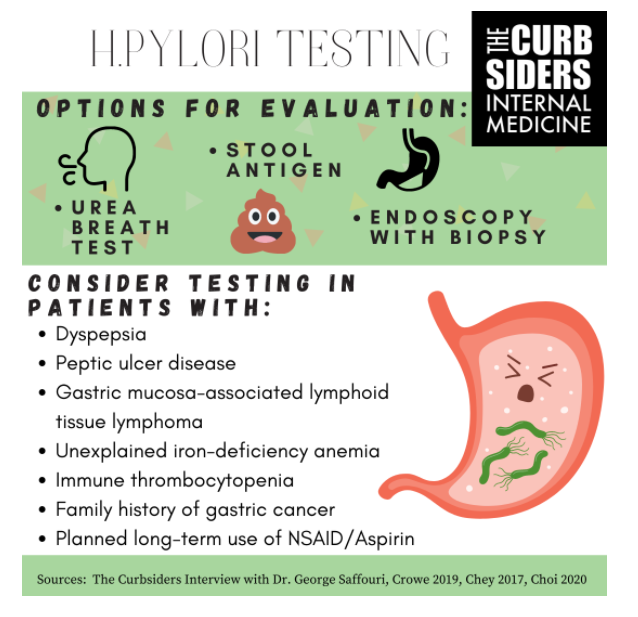
H. pylori is classified as a carcinogen by the WHO with a clear causal cancer link (IARC 1994). Patients who should be tested for H. pylori include patients with dyspepsia, peptic ulcer disease, gastric mucosa-associated lymphoid tissue lymphoma (MALToma), unexplained iron-deficiency anemia, immune thrombocytopenia, and patients with early gastric cancer who undergo endoscopic resection(Crowe 2019, Chey 2017). Pathophysiology of the immune thrombocytopenia/H. pylori connection is not well-understood.
Family history of gastric cancer is a group to consider as well, as emerging evidence shows that eradication may reduce risk of development of gastric cancer in these individuals (Choi 2020). Some evidence also exists for testing of H. pylori in patients requiring long-term aspirin/NSAIDs (Crowe 2019, Chey 2017).
Approach screening with a mindset of global and cultural competence. While H. pylori is reported as ‘low prevalence’ in the United States, other global regions have higher prevalence. As such, some guidelines recommend screening in first-generation immigrants from high prevalence countries (El-Serag 2018).
Additionally, certain patient groups (who are traditionally classified by racial/ethic group, although we believe this is a flawed categorization, Vyas 2020) have higher prevalence of H. pylori, including patients who identify as Hispanic or African American (El-Serag 2018, Epplein 2011, Huerta-Franco 2018). Racism and social determinants of health impact prevalence in certain socioeconomic groups as well as influence treatment and management of dyspepsia. For example, Black Americans are less likely to receive eradication testing in H. pylori management (Reichstein 2020). Undetected H. pylori infection may also be associated with increased risk of colon malignancy in Black patients (Butt 2019).
How to Test
Don’t use serologies for H. pylori, ast these do not distinguish between active and previous infection per Dr. Saffouri. The non-invasive options (Crowe 2019, Chey 2017) for evaluating H. pylori infection include:
-Urea breath test
-H. pylori stool antigen test
Best way to test invasively would be endoscopy with a biopsy (Crowe 2019, Chey 2017) and histopathological assessment or rapid urea test of biopsy.
Treatment & Counseling
Patients should be reassured that this is a common infection per Dr. Saffouri. There is evidence that the infection commonly is acquired in childhood (Kavitt 2017). Dr. Saffouri advises that it is important to emphasize that this infection, while treatable, requires strict adherence to the treatment regimen and it can have some associated side effects (nausea, vomiting, diarrhea). He impresses upon patients, the severity of the infection as well as cancer link and why taking all the meds is really crucial.
Which Regimen?
Triple therapy with a combination of clarithromycin, amoxicillin (or metronidazole if true penicillin allergy), and PPI is NOT the appropriate go-to regimen anymore, due to increased global H. pylori resistance to clarithromycin (Huang 2017).
Best regimen is bismuth-based quadruple therapy (bismuth + PPI + tetracycline + metronidazole) (Huang 2017, Chey 2017). Tetracycline may be replaced with doxycycline if needed per Dr. Saffouri/Guidelines (Chey 2017). Use of clarithromycin is only recommended if you know your local resistance profile (Chey 2017) which per Dr. Saffouri is not easily available information. Unfortunately, the quadruple therapy is not well-tolerated in Dr. Saffouri’s expert opinion due to the side effect profile and frequent dosing.
Saffouri’s Recommendations for Antibiotics:
- Possible second-line regimen should be different from the first-line!
- Do not use similar antibiotic classes!
- The biggest reason a treatment regimen will fail a patient is due to antibiotic resistance.
A second-line for Dr. Saffouri usually includes levofloxacin. A meta-analysis showed that levofloxacin regimens may provide superior eradication (Rokkas 2021), although there is increasing overall fluoroquinolone resistance (Dalhoff 2012) and they have a poor side effect profile (FDA 2018). However, if the patient continues to test positive for H. pylori after completion of the quadruple bismuth therapy, Dr. Saffouri will try levofloxacin + PPI + amoxicillin.
Kashlak Pearl: Take a thoughtful assessment of antibiotic allergy history and consider testing for penicillin allergy! 10% of the U.S. population report penicillin allergies but less than <1% of the population are allergic when tested (CDC 2016) and being able to take this antibiotic class can open up a huge important range of therapeutic options for many infections, H. pylori included!
Eradication Testing, Recurrence, and New Drugs on The Horizon
All patients who have tested positive for H. pylori and undergone a course of treatment should undergo eradication testing to ensure success of treatment (Chey 2017) which can be either a stool antigen test or a urea breath test. It occurs 4 weeks after completion of regimen, and if positive you should initiate a second-line or third-line therapy (Shah 2021).
New treatment vonoprazan (a potassium blocker) may become standard of care, some studies are showing superior efficacy in eradication of H. pylori infection.
Once it is eradicated, it is usually gone for good. The recurrence rate is only 1-2% (Nam 2019, Xue 2019) per year. May consider re-testing if the patient has confirmed eradication and then returns with similar symptoms, per Dr. Saffouri, but this is not a common scenario. Unfortunately, while some do experience improvement in symptoms (Lane 2006, Tsuda 2020), dyspepsia commonly recurs after H. pylori eradication (di Mario 2005).
Take Home Points
- Remember H. pylori is a carcinogen! It is a causative agent in gastric cancer and if found it needs to be treated, with confirmation of eradication.
- Avoid H. pylori serologies for identification of the organism, you want to stick to stool antigen, urea breath test, or endoscopy with biopsy.
- Do not use clarithromycin triple therapy! Choose quadruple therapy.