The JACC article referenced today is an awesome brief review of heart failure guidelines.
In this post I link to and excerpt from ACC/AHA Versus ESC Guidelines on Heart Failure [PubMed Abstract] [Full Text HTML] [Download Full Text PDF]. JACC VOL. 73, NO. 21, 2019 van der Meer et al. JUNE 4, 2019:2756 – 6 8
All that follows are excerpts from the above article.
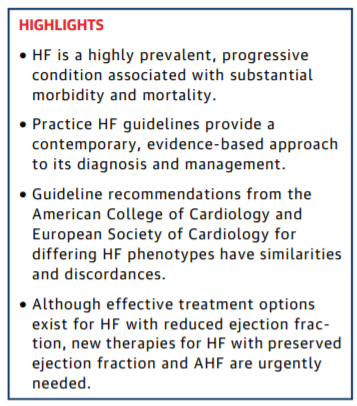
Abstract
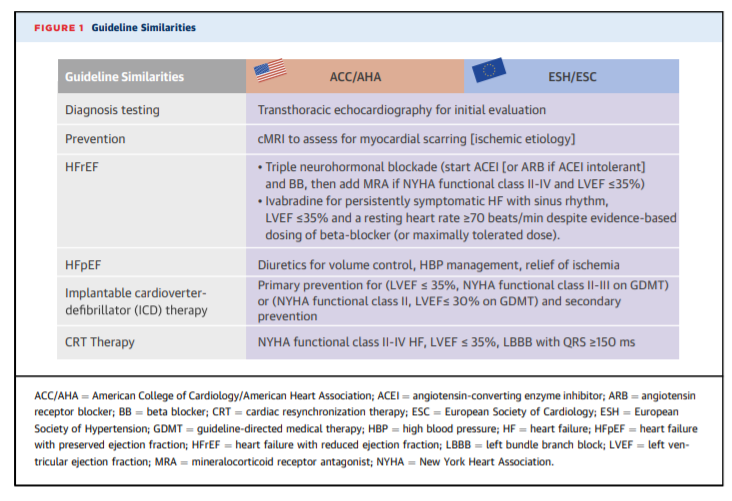
The 2013 (with updates in 2016 and 2017) American College of Cardiology/American Heart Association and 2016
European Society of Cardiology guidelines provide practical evidence-based clinical guidelines for the diagnosis and
treatment of both acute and chronic heart failure (HF). Both guidelines address noninvasive and invasive testing to
establish the diagnosis of HF with reduced ejection fraction and HF with preserved ejection fraction. Extensive trial
evidence supports the use of guideline-directed medical therapy and device-based therapies for the optimal management
of patients with HF with reduced ejection fraction. Specific recommendations are also provided for HF with preserved
ejection fraction although the evidence is substantially weaker. Management of medical comorbidities is now addressed
in both guidelines. Acute HF and end-stage disease requiring advanced therapies are also discussed. This review compares
specific recommendations across the spectrum of HF phenotypes and disease severity, highlights areas where differences
exist, and lists consequential studies published since the latest guidelines. (J Am Coll Cardiol 2019;73:2756–68)
© 2019 by the American College of Cardiology Foundation.CLASSIFICATIONS OF DISEASE: BACKGROUND
The clinical syndrome of HF may result from disorders of the pericardium, myocardium, endocardium, or heart valves. However, most patients have symptoms related to impaired LV myocardial function. Abnormalities of systolic and diastolic function coexist, irrespective of ejection fraction. LV ejection
fraction (LVEF) remains crucial in classification because it was originally used to differentiate HFrEF and evaluate its pathophysiology and response to therapy. Clinical trials that have demonstrated a mortality benefit have been in this population. HFrEF is defined by clinical HF syndrome with LVEF ≤40%, whereas HFpEF encompasses HF patients with
LVEF ≥50%. ESC criteria require additional supportive findings beyond signs or symptoms of HF and include elevated levels of natriuretic peptide, and objective evidence of structural or functional alterations. Key structural abnormalities include left
atrial enlargement or increased LV mass; functional alterations consistent with diastolic dysfunction including E/e’ >13 and a mean e’ septal and lateral wall <9 cm/s (5). A third group has been recently characterized—HF with mid-range ejection fraction (HFmrEF) (LVEF = 40% to 49%).
PREVENTIVE STRATEGIES
ASYMPTOMATIC LV DYSFUNCTION/STAGE B DISEASE
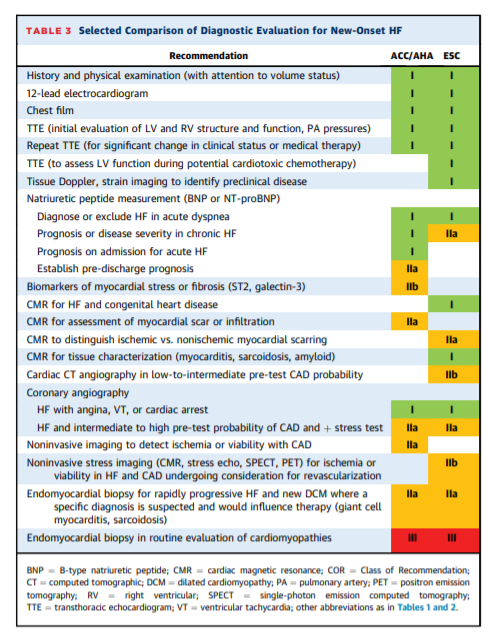
DIAGNOSTIC EVALUATION
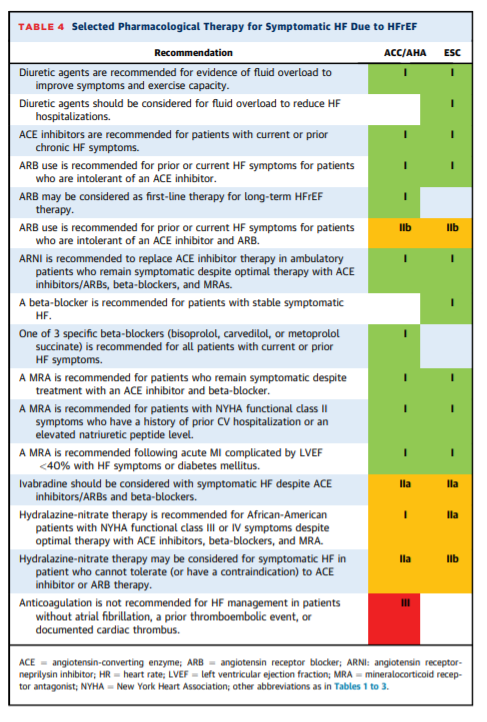
PHARMACOLOGICAL TREATMENT HFrEF
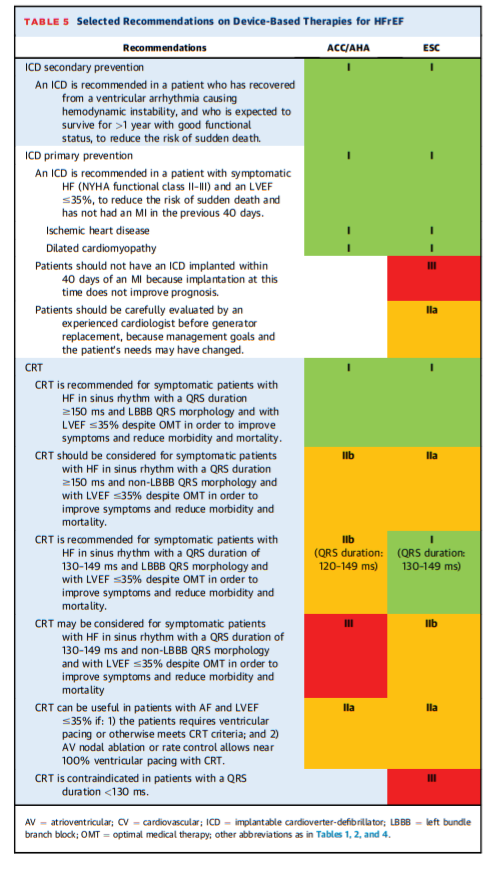
DEVICE-BASED THERAPIES
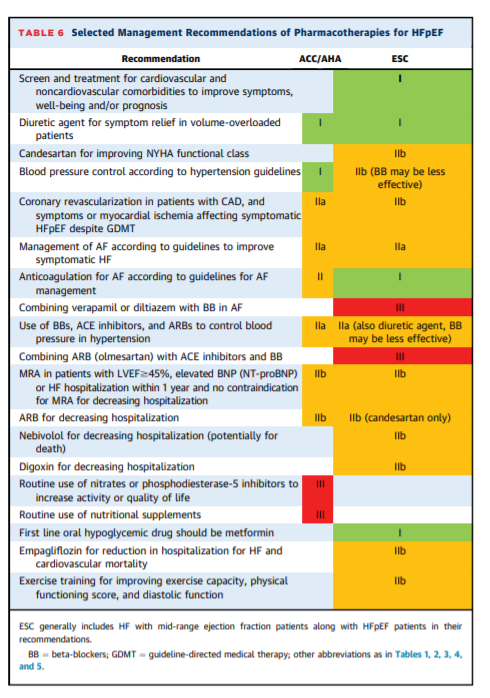
PHARMACOLOGICAL TREATMENT OF HFpEF
SELECTED COMORBIDITIES AND HF
start here