Today, I review, link to, and excerpt from Computed tomographic angiography in coronary artery disease [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. EuroIntervention. 2023 Apr 3;18(16):e1307-e1327. doi: 10.4244/EIJ-D-22-00776.
All that follows is from the above resource.
Abstract
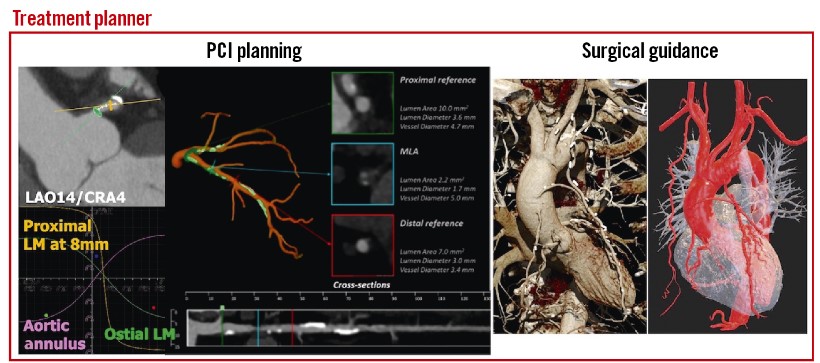
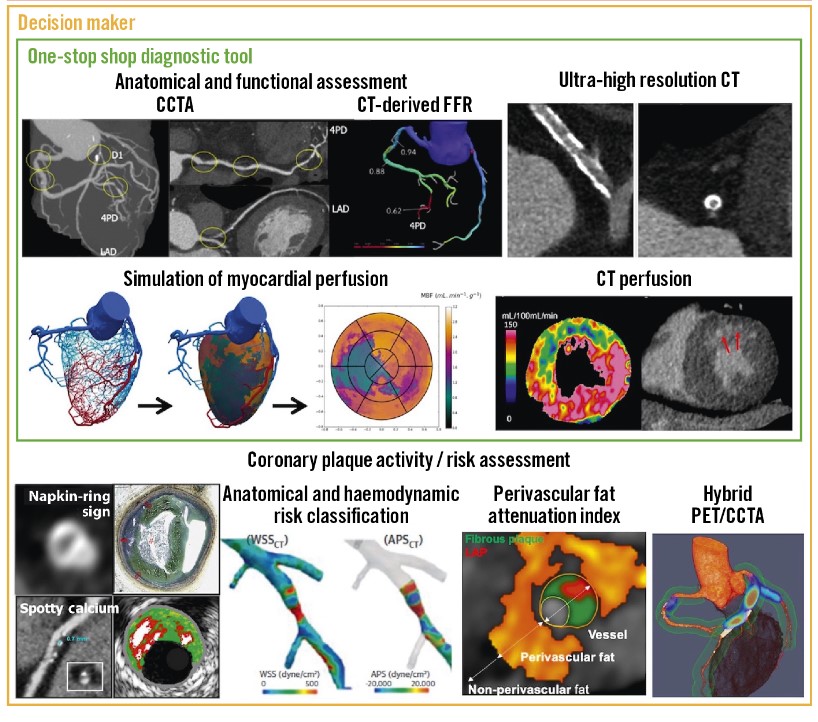
Coronary computed tomographic angiography (CCTA) is becoming the first-line investigation for establishing the presence of coronary artery disease and, with fractional flow reserve (FFRCT), its haemodynamic significance. In patients without significant epicardial obstruction, its role is either to rule out atherosclerosis or to detect subclinical plaque that should be monitored for plaque progression/regression following prevention therapy and provide risk classification. Ischaemic non-obstructive coronary arteries are also expected to be assessed by non-invasive imaging, including CCTA. In patients with significant epicardial obstruction, CCTA can assist in planning revascularisation by determining the disease complexity, vessel size, lesion length and tissue composition of the atherosclerotic plaque, as well as the best fluoroscopic viewing angle; it may also help in selecting adjunctive percutaneous devices (e.g., rotational atherectomy) and in determining the best landing zone for stents or bypass grafts.
Introduction
CAD phenotypes may be viewed as a pyramid of multiple layers of increasing anatomical complexity3. At the bottom are subjects with normal epicardial conductance vessels who have no atherosclerotic plaque and an excellent prognosis. Above them are patients with non-obstructive coronary plaque who have an increased risk of myocardial infarction (MI) and next, patients with progressive increases in plaque burden. Patients with normal coronary arteries or non-obstructive plaque may have structural or functional coronary microvascular dysfunction (CMD) that can lead to anginal symptoms with its two corollary syndromes (INOCA and ANOCA, i.e., ischaemia/angina with non-obstructive coronary arteries). Notably, “evidence of impaired coronary microvascular function should be present” with or without ischaemia4.
PRETEST PROBABILITY FOR OBSTRUCTIVE CAD AND DIAGNOSTIC CCTA
The application of the pretest probability (PTP) for significant obstructive CAD (as determined by invasive coronary angiography [ICA] and fractional flow reserve [FFR]) based on age, sex, and the nature of symptoms underwent a major revision in the 2019 European Society of Cardiology (ESC) Guidelines for the diagnosis and management of chronic coronary syndromes (CCS)5.
The PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) trial showed that in patients with a PTP <15%, the annual risk of cardiovascular death or MI was <1%6. The SCOT-HEART (Scottish Computed Tomography of the Heart) trial confirmed that the 2019 ESC estimates of PTP based on ICA and FFR were broadly similar to the prevalence observed on CCTA in the trial cohort7, although it tended to underestimate the real prevalence, or alternatively, CCTA might overestimate the CAD (Supplementary Figure 2A)*. The rates of 5-year cardiac death or non-fatal MI were 4.1%, 1.5% and 1.4% in patients with a PTP >15%, 5-15% and <5%, respectively (p<0.001 between groups) (Supplementary Figure 2B)*.
*To see all the Supplementary Figures, download the PDF. The link to download the PDF is in the Full-Text HTML.
On the other hand, the results of the Western Denmark Heart Registry, including 23,759 symptomatic patients, challenge the traditional dichotomous definition of CAD as “obstructive” or “non-obstructive” for identifying truly high-risk patients8. Major adverse cardiac events (MACE; MI, stroke, and all-cause death) at 4-year follow-up increased stepwise with both higher coronary artery calcium (CAC) scores and the number of vessels with obstructive disease detected by CCTA. Of note, when stratified into 5 groups according to CAC scores, the presence of obstructive CAD was not associated with a higher risk of MACE than the presence of non-obstructive CAD (NOCAD)8.
STRUCTURED REPORTING SYSTEM FOR CCTA
This year, the expert document 2022 Coronary Artery Disease-Reporting and Data System, or CAD-RADS 2.0, expanded on its first version, which was published in 2016 as a multi-society sponsored statement from the Society of Cardiovascular Computed Tomography (SCCT)/ACC/American College of Radiology (ACR)/North American Society of Cardiovascular Imaging (NASCI) to standardise the reporting system for patients undergoing CCTA and to guide the possible next steps in patient management10. One key update provided in the CAD-RADS 2.0 statement is the estimation of coronary plaque burden; this is due to the emerging data supporting its stronger prognostic value over merely the presence or absence of an anatomical stenosis. In addition, there was a focus on physiological assessments of lesion-specific ischaemia using CT-derived FFR (FFRCT) or CT perfusion (CTP).
The CAD-RADS score stratifies CAD stenosis severity as 0 (0%), 1 (1-24%), 2 (25-49%), 3 (50-69%), 4A (70-99% in 1 to 2 vessels), 4B (70-99% in 3 vessels or ≥50% in the left main), or 5 (100%). The additional description of P1 to P4 are used to indicate increasing categories of plaque burden. In the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry, stratifying 5,039 patients without known CAD by CAD-RADS scores, a multivariable Cox model demonstrated that CAD-RADS scores were strongly associated with an elevated risk for death or MI, with hazard ratios (HR) ranging from 2.46 for CAD-RADS 1 to 6.09 for CAD-RADS 5, using CAD-RADS 0 as the reference group (p<0.0001 for all comparisons)11. The prognostic implications of the CAD-RADS reporting system might be of no surprise since the CAD-RADS score was designed to reflect CAD severity, therefore it is no wonder that it is associated with outcome.
The Coronary Artery Calcium Data and Reporting System (CAC-DRS) aimed at communicating the findings of CAC scanning on all non-contrast CT scans to facilitate clinical decision-making, with recommendations for subsequent patient management12. The CAC-DRS classified CAC based on Agatston scores as 0 (Agatston score 0), 1 (1-99), 2 (100-299), and 3 (≥300), as well as on visual assessment. In the SCOT-HEART trial assessing 1,769 patients, patients classified as CAC-DRS 3 were at an increased risk of fatal or non-fatal MI compared to CAC-DRS 0 patients (HR 9.41, 95% confidence interval [CI] 3.24-27.31; p<0.001)13.
Ultimately these structured reporting systems allow accurate communication of patient findings and convey prognosis, which may help provide guideline-based care directly from the CCTA findings.
RULING OUT CAD
Prospective multicentre studies investigating the diagnostic accuracy of CCTA for detecting a narrowing in an epicardial vessel in patients with suspected but unproven CAD have reported sensitivities of 85%-99% and specificities of 64%-92% (Supplementary Table 1)1. In a meta-analysis reported by Knuuti et al, when anatomical coronary narrowing >50% on ICA was considered a reference standard, CCTA had a sensitivity of 97%, a specificity of 78%, and substantial positive and negative likelihood ratios (4.44 and 0.04, respectively)14 (Supplementary Figure 3). Recent technological advancements have improved the diagnostic accuracy for detecting a significant coronary artery stenosis (≥50%), even in patients with atrial fibrillation and/or high heart rates, and photon-counting CT or ultra-high spatial resolution CT (UHR-CT) may further boost image resolution with inherent spectral information (Supplementary Table 1)1516.
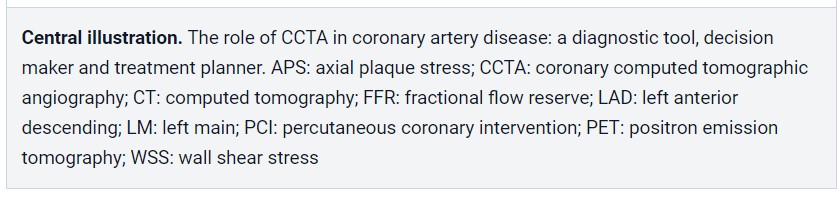
UHR-CT provides a resolution of 150-200 μm and allows improved visualisation of calcified, stented, or small-diameter vessels17 (Figure 1).
Using a commercially available UHR-CT, a recent study of high-risk patients with severe CAD as well as very high calcium scores (mean CAC score 1,205) provided promising preliminary data demonstrating a high diagnostic accuracy with a specificity of 88% in a per-vessel analysis compared with ICA (Supplementary Table 1)15. FFRCT is helpful in improving the dismal specificity of standard CCTA but does not improve the sensitivity of the technique. With the advent of UHR-CT, a significant reduction in false-positive findings may be expected and supersedes the need for an additional functional evaluation such as FFRCT. Therefore, in this new era, the clinical role of FFRCT will have to be re-evaluated18.
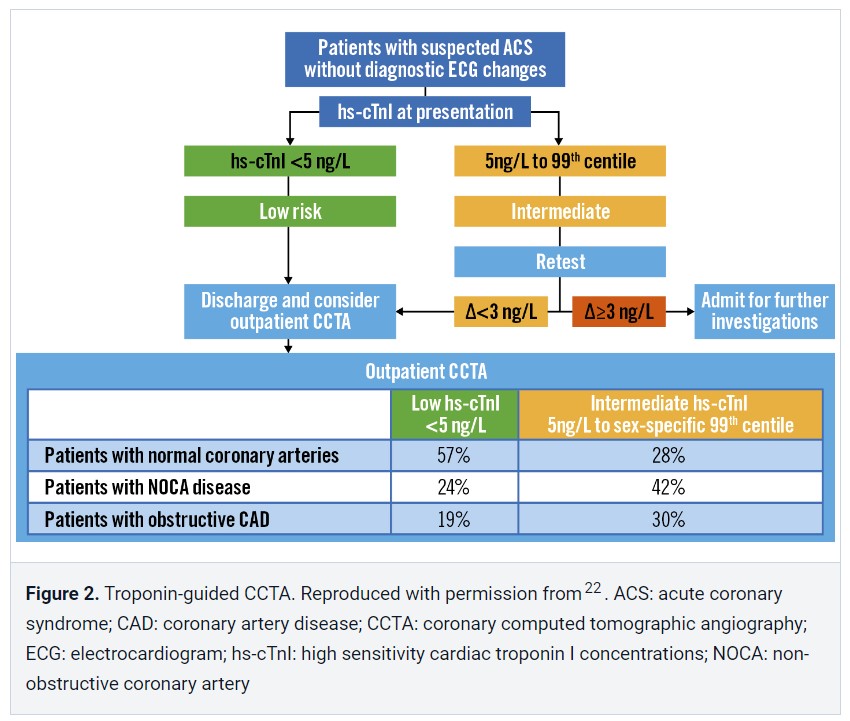
In a prospective cohort study of 250 patients presenting to the emergency department, troponin-guided CCTA was evaluated in patients with suspected acute coronary syndrome (ACS) but a high-sensitivity cardiac troponin I concentration below the sex-specific 99th percentile – thus, after excluding non-ST-segment elevation MI (NSTEMI)22. This approach to using cardiac troponin to select patients for downstream CCTA after NSTEMI has been ruled out has the major potential to improve patient outcomes by accurately diagnosing CAD and guiding preventative treatments (Figure 2).
NON-INVASIVE FUNCTIONAL IMAGING: FFRCT AND MYOCARDIAL PERFUSION IMAGING
Diagnostic strategies to accurately rule out patients who do not require further testing are needed to offset the potentially higher ICA utilisation after CCTA as the first-line diagnostic workup26. Thus, guidelines recommend second-line function testing if CCTA suggests CAD of uncertain functional significance5.
FFRCT – unlike MPI with SPECT/PET – is based on standard CCTA images from which patient-specific 3-dimensional (3D) anatomical and physiological models are derived, without the need for additional testing, medication, or radiation.
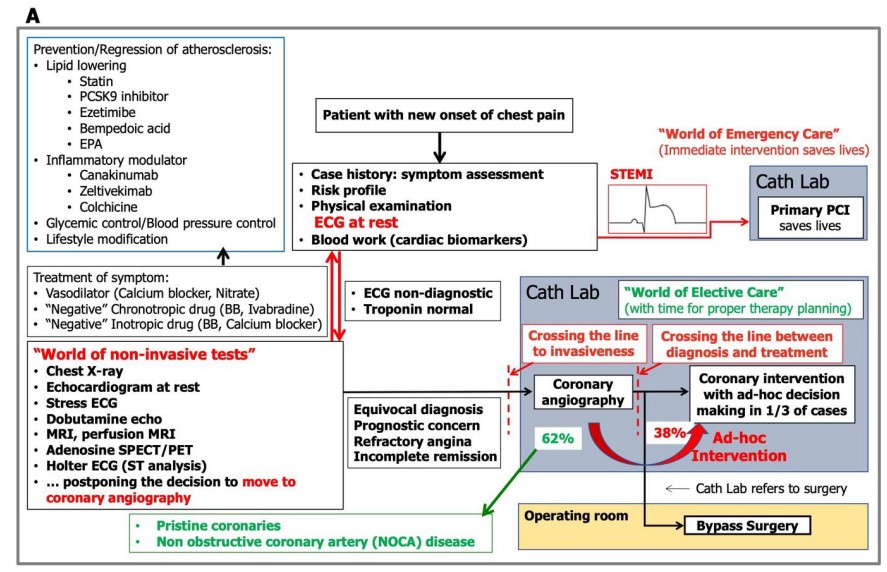
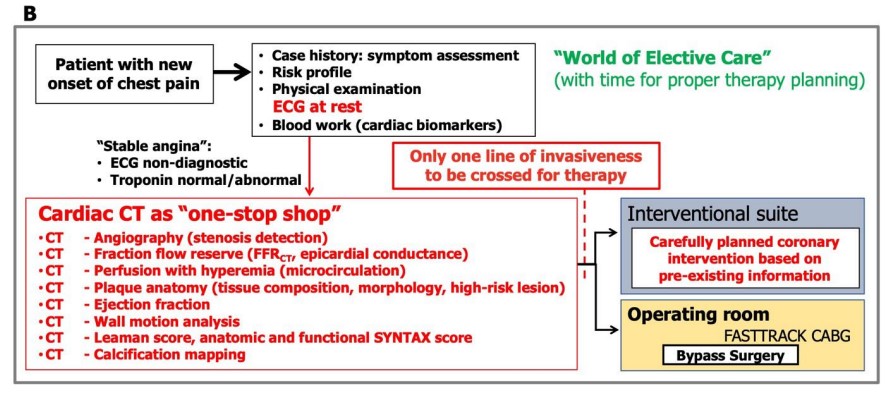
In the 2019 ESC Guidelines, CCTA with non-invasive functional imaging was given a class I level of evidence B recommendation as the initial test to diagnose CAD in symptomatic patients in whom obstructive CAD could not be excluded by clinical assessment alone5. In the recent ACC/AHA Chest Pain guidelines, CCTA received a class 2a recommendation for “determining atherosclerotic plaque burden and progression to obstructive CAD, and guiding therapeutic decision-making”. FFRCT was recommended (class 2a) down to the level of a 40% stenosis for the “diagnosis of vessel-specific ischaemia and to guide decision-making regarding the use of ICA”9. The forthcoming clinical use of CCTA as a “one-stop shop”, including anatomical and physiological assessment to diagnose patients with new-onset chest pain (Supplementary Figure 5), is also expected to serve as a decision-making tool.
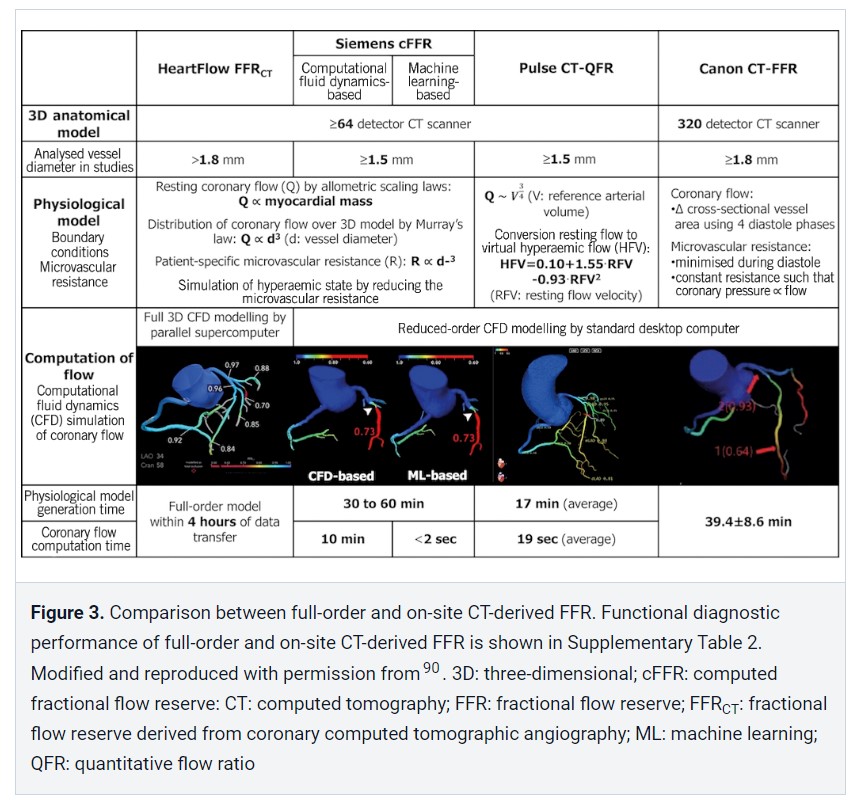
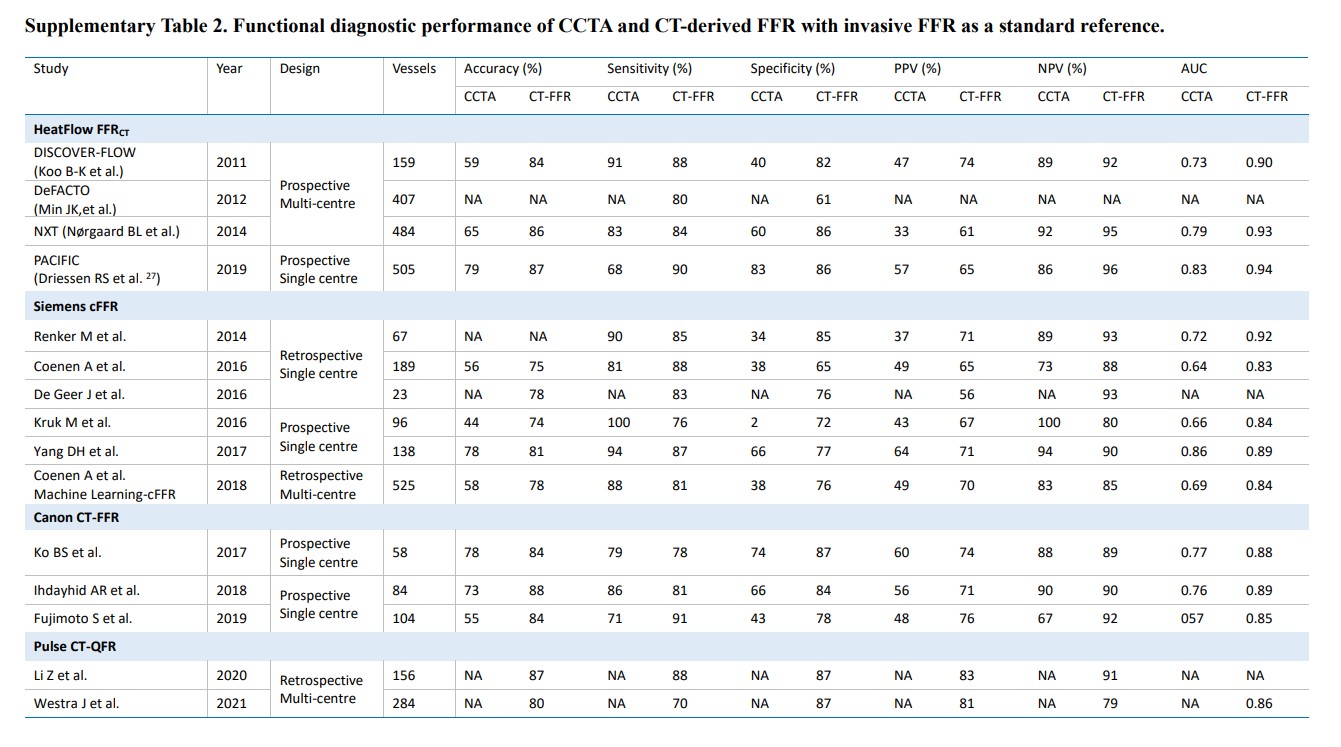
Recently, there has been increasing interest in alternative, less demanding computational approaches that allow for on-site analysis. Comparisons of physiological models, computation time, and diagnostic performance between full-order and on-site CT-derived FFR are shown in Figure 3 and Supplementary Table 2.
CT PERFUSION
FFRCT benefits from the fact that analyses can be performed straight from the CCTA acquisition without additional scanning and pharmacological stressors; however, its diagnostic value in patients with previous MI, stents or bypasses remains to be established2634. MPI including CTP remains a valuable alternative, although CTP is not used as a routine diagnostic tool in current clinical practice2535.
A meta-analysis of 54 articles and 5,330 patients indicated that CTP and its combined use with CCTA yielded a higher diagnostic performance (sensitivities 83% and 89%; specificities 79% and 81%, respectively) compared to CCTA alone, with an invasive FFR ≤0.80 as a standard reference36.
The two primary methods of acquisition are static CTP and dynamic CTP with rest CCTA scanning followed by pharmacological stress or vice versa37.
The two primary methods of acquisition are static CTP and dynamic CTP with rest CCTA scanning followed by pharmacological stress or vice versa37.
STATIC STRESS CTP
Although both technologies of CTP and FFRCT are based on CT imaging, allowing anatomical and functional – perfusion or physiology – evaluation within 1 modality, CTP assesses the effects of both epicardial and microvascular perturbation, which is a different level of the ischaemic cascade from FFRCT34. In the PERFECTION (PERfusion Versus Fractional Flow Reserve CT Derived In Suspected CoroNary) study, the AUC to detect flow-limiting stenoses with CCTA, CCTA+FFRCT, and CCTA+static stress-CTP were 0.89, 0.93, 0.92, respectively, in a vessel-based model, with significant additional values for CCTA+FFRCT and CCTA+static stress-CTP versus CCTA alone (p<0.001) but no difference between CCTA+FFRCT versus CCTA+static stress-CTP39.
The Core320 (Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320 Detector Computed Tomography) study compared the prognostic value of a combined anatomical/functional assessment by non-invasive imaging versus a traditional approach, showing that 5-year MACE (cardiac death, MI, hospitalisation for chest pain or congestive heart failure, and late revascularisation)-free survival rates were greater among patients with normal findings of combined CCTA-CTP compared to ICA-SPECT: 85% vs 80% (95% CI for difference: 0.1-11.3)40.
DYNAMIC CTP
[See article]
Regardless of the CTP acquisition mode, the SCCT consensus document underlined the importance of patient selection and recommended adding CTP to CCTA when patients were at high atherosclerotic risk for obstructive CAD, including those with prior coronary intervention or significant calcification, or when there is a stenosis of indeterminate functional significance37. It also needs to be reassessed whether CTP with its associated radiation burden, in addition to CCTA, is still necessary when the use of UHR-CT, with a significant reduction in false-positive findings, will be more generalised in practice. Alternatives such as stress echocardiography or stress CMR perfusion imaging may be considered.
NOCAD AND MICROVASCULATURE DYSFUNCTION
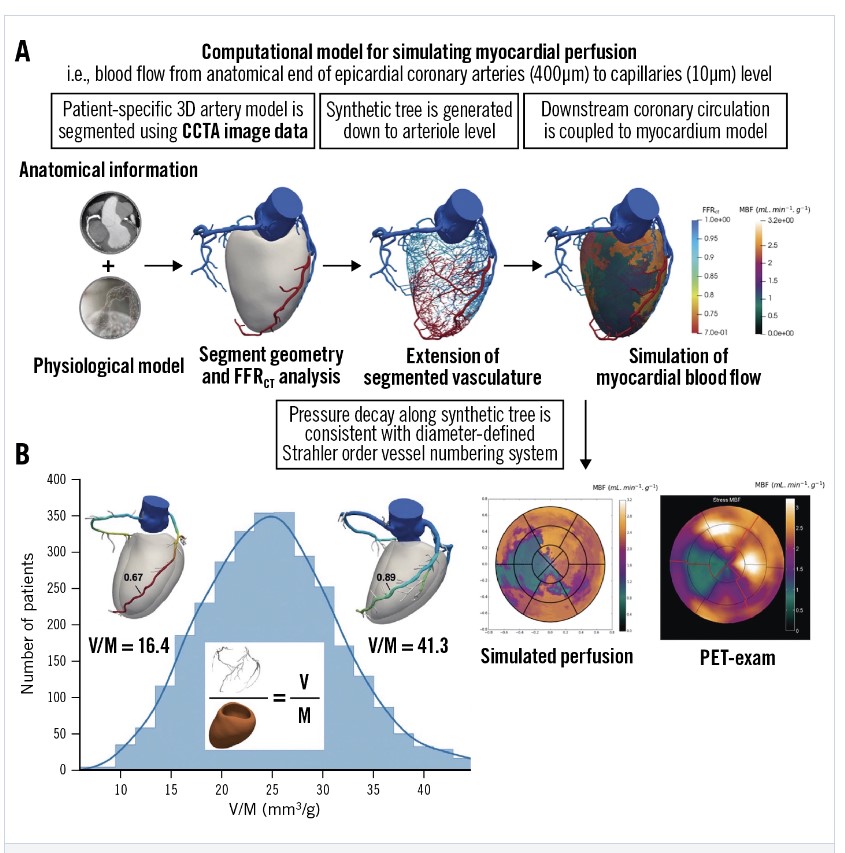
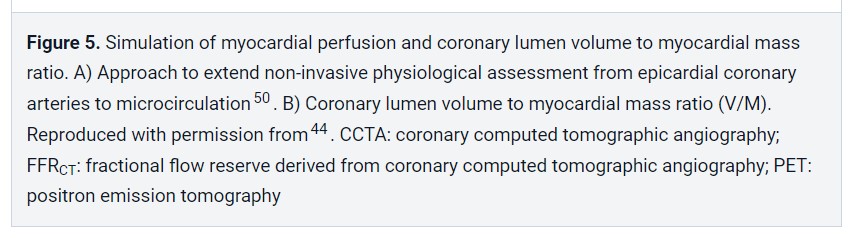
Current explanations for INOCA reference either CMD or vasospastic angina, while in contrast, the recent US guidelines advocate ruling out the functional significance of diffuse atherosclerosis. Another independent explanation for INOCA is that it is related to the coronary lumen volume to myocardial mass ratio (V/M), measured non-invasively using CCTA. V/M provides an integrated measure of the balance between myocardial blood supply capacity and demand in vivo44 (Figure 5).
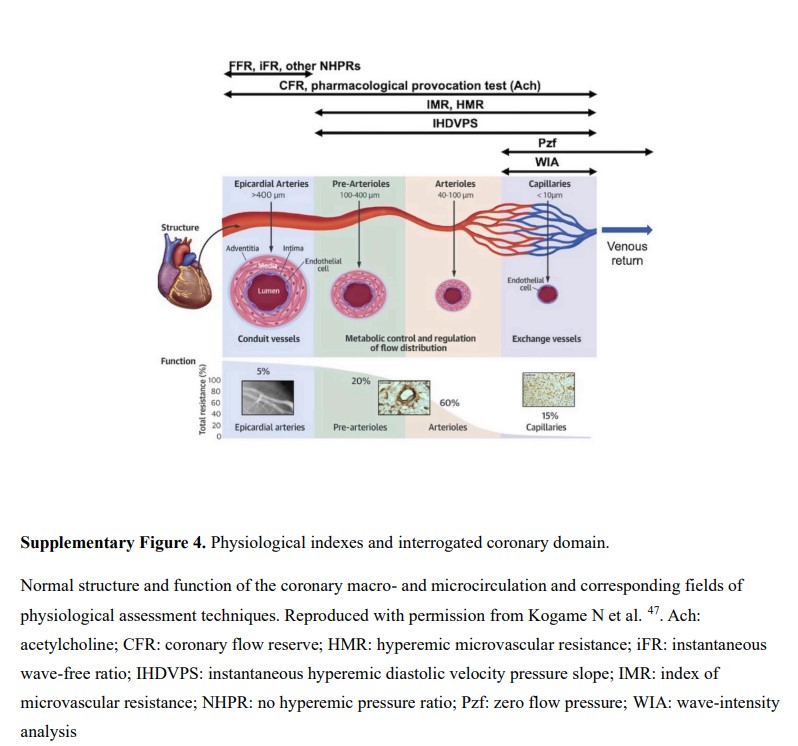
Epicardial arteries, visualised by the “clinical angiographer”, represent only 5% of the volume of the coronary tree, while pre-arterioles, arterioles, and capillaries represent 95% of the remaining coronary volume (Supplementary Figure 4).
The epicardial arteries (>400 μm) are the conduit vessels and might be interrogated by FFR, instantaneous wave-free ratio (iFR), and other non-hyperaemic pressure ratios47. The pre-arterioles (100-400 μm) and arterioles (40-100 μm) are involved in the regulation of flow distribution and in metabolic control, and the capillaries (<10 μm) are exchange vessels48.
One approach to extend non-invasive physiological assessment from the epicardial coronary arteries to the microcirculation is to generate a synthetic tree following branching laws from the CCTA data down to the microvasculature. Recently, an algorithm for the generation of patient-specific cardiac vascular networks starting from segmented epicardial vessels down to the arterioles has been developed, with the potential to advance the non-invasive CCTA modelling of coronary flow, microvascular function, and myocardial perfusion4449. Papamanolis et al have described a computational model for simulating myocardial perfusion, i.e., blood flow from the anatomical end of the epicardial coronary arteries (400 μm) to the level of the capillaries (10 μm) (Figure 5)50.
In this proof-of-concept paper, simulated MBF demonstrated favourable comparisons to [15O]H2O PET data in five patients with NOCAD and in one patient with severe obstructive disease for both resting and hyperaemic conditions.
SCAPIS (Swedish Cardiopulmonary Bioimage Study) recruited 30,154 randomly invited individuals aged 50 to 64 years who were not known to have CAD and had high-quality CCTA, showing that silent coronary atherosclerosis was common (42.1%), significant stenosis (≥50%) was less common (5.2%), and more severe forms, such as left main, proximal left anterior descending artery or 3VD, were rarely found (1.9%) in a middle-aged population53. In addition, CCTA-detected atherosclerosis increased with an increasing CAC score: all those with CAC >400 had atherosclerosis, of whom 45.7% had significant stenosis; 5.5% of those with 0 CAC had atherosclerosis, of whom 0.4% had significant stenosis, with increasing prevalence at higher baseline risk.
The ACC/AHA guidelines on the primary prevention of cardiovascular disease recommend (IIa) measuring the CAC score to guide the clinician-patient risk discussion – not as a screening test – “in adults at intermediate risk, if risk-based decisions for preventive interventions remain uncertain”, with the emphasis that the absence of CAC does not rule out non-calcified plaque, and that clinical judgment about risk should prevail51. Indeed, SCAPIS showed that in the population with 0 CAC, CCTA-detected atherosclerosis was present in 6.0% of patients with a strong family history of MI, 6.8% of those who were currently smokers, and 8.1% of those with diabetes53.
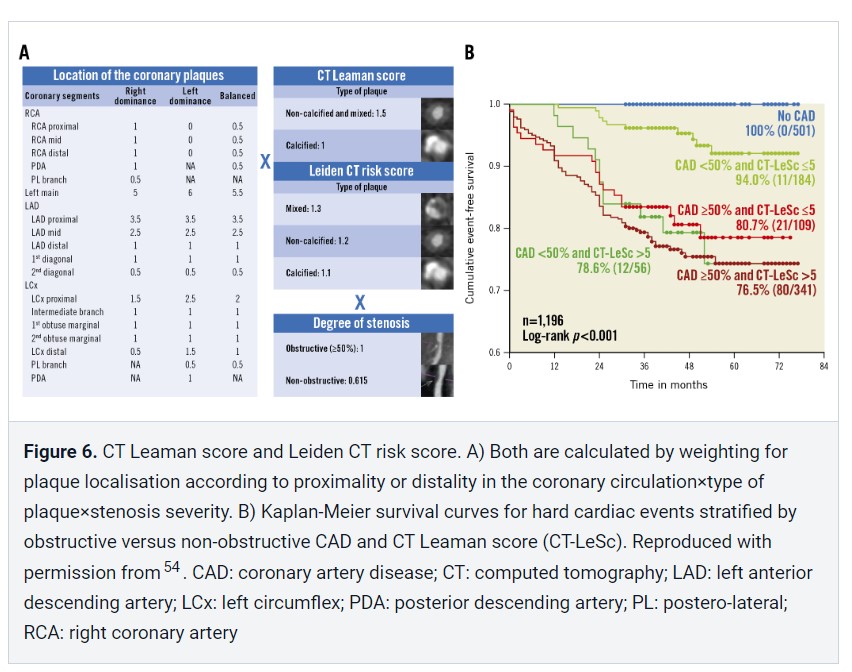
In 2015 – prior to the 2022 CAD-RADS 2.0 statement, which focuses on the estimation of coronary plaque burden in addition to the severity of stenosis due to its strong association with incident coronary heart disease events10 – the CT-adapted Leaman score (CT-LeSc), developed to quantify CCTA information about atherosclerotic burden (lesion localisation, degree of stenosis, and plaque composition), was validated as an independent long-term predictor of hard cardiac events54 (Figure 6).
Patients with NOCAD and a CT-LeSc >5 had a similar risk of cardiovascular events when compared to patients with obstructive CAD (>50% stenosis) but a CT-LeSc <554. In the CONFIRM registry, the 5-year prognostic value of the CT-LeSc was significant in patients without obstructive stenosis55. The Leiden group slightly modified the Leaman score by adding the subcategory “mixed plaque”, in addition to calcified and non-calcified plaque56 (Figure 6). A higher Leiden CCTA risk score was associated with 5-year all-cause mortality or MI in the derivation (Leiden University Medical Center) and external validation cohort (the CONFIRM registry)156.
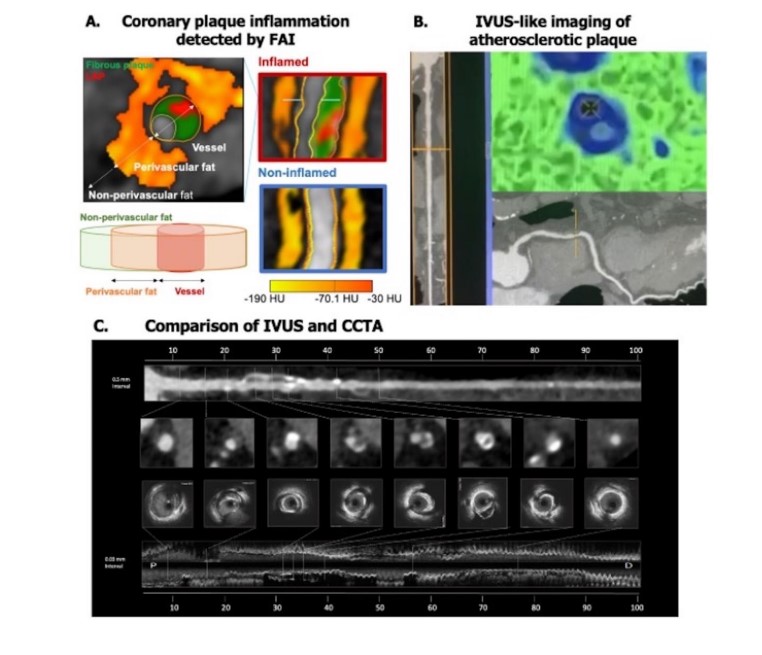
It is noteworthy that most ACSs are caused by unstable but non-obstructive atherosclerotic plaque which cannot be identified by current invasive or non-invasive diagnostic tests detecting coronary luminal stenosis or stress-induced myocardial ischaemia57. The CRISP-CT (Cardiovascular RISk Prediction using Computed Tomography) study validated the prognostic role of the perivascular fat attenuation index (FAI), the first non-invasive biomarker of CCTA-detected “coronary inflammation”, which is a driver of coronary atherosclerosis plaque formation and is a typical feature of plaque rupture, leading to ACS57. High perivascular FAI values (cut-off ≥−70.1 Hounsfield units [HU]) identify high-risk individuals with a 5- to 9-fold higher adjusted risk for cardiac death and, therefore, could guide early targeted primary prevention and intensive secondary prevention (Supplementary Figure 6A).
HYBRID CCTA AND MOLECULAR PET
Start here.