In this post I link to and excerpt from EMCrit 267 – They are not All Right!! An interview on Hemodynamic Assessment with Mike Patterson. March 6, 2020 by Scott Weingart, MD FCCM
All that follows is from the above.
Michael Patterson FCICM FANZCA
Mike is an intensivist anaesthetist in Melbourne. He has spent years thinking about disasters seen in anaesthetics and ICU–most of them are hemodynamic ones. His original interest in this problem stemmed from the death of a young lady having elective gynae surgery, in the setting of anaphylaxis. She had an easily palpable central pulse and reassuring EtCO2 throughout. He was involved late due to issues with arterial access. She died of a hypoxic brain injury solely because her pressure was too low for too long. He has been reflecting on this over the last few years and building up a picture of the problems and the solutions. Subsequently, he had been involved in one patient that died in the setting of a POCUS pulse but inadequate pressure and another young lady who lived despite nearly the same problem occurring as the lady that died.
Central pulses are almost meaningless
– We are mostly just feeling a change in pressure
– Hence 50/10 might feel similar to 120/80
Central pulses are particularly dangerous in distributive shock where the pulse will be felt strongly below 50/-. This has been my repeated experience. It is easily palpable even in hypovolaemic shock with BP < 60 on occasion – You can’t measure pressure from a central pulse until you place an arterial line.
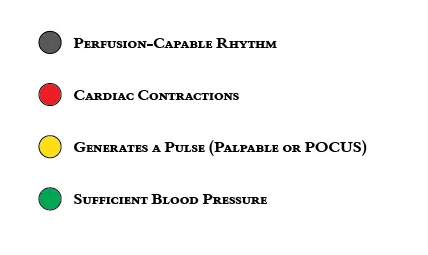
The problems with ROSC in the setting of PEA or profound hypotension in general are:
POCUS pulse has the same problems as a central pulse unless applied to the brachial artery where you can place a manual cuff and visualize the occlusion pressure.
Normal EtCO2
A normal EtCO2 is not reassuring that the pressure is adequate, as you mention – It is useful to suggest ROSC when it kicks up – It is dangerous as any reassurance in distributive shock where pulmonary perfusion is maintained and EtCO2 often doesn’t drop at all despite BP’s < 50/- – In the cardiac arrest setting, PaCO2 has often risen significantly so an EtCO2 in the 30’s may still represent inadequate perfusion let alone pressure I like your step-wise summary of the progression to ROSC. It is brilliant.
Radial Pulse?
Identify that the radial pulse is rapidly and easily felt before you have a problem – This is obviously irrelevant for those presenting in cardiac arrest – In most other circumstances, if you knew it was strong and easily palpable prior, you can’t end up with confirmation bias – convincing yourself there is no problem. Occasionally it is difficult to locate prior, in which case, if they are sick you better put in an arterial line while the going is good as you are hosed with no endpoint. – It is essential in anaesthesia where patients are well before we start.
Peri-Intubation A-Line
But it is useful for peri-intubation management in ED and ICU when there is no arterial line – If it disappears – you have a problem until you get it back. No denial. – Once you have it – you can measure a manual BP rapidly – I agree that people don’t feel pulses well in cardiac arrest. It needs to match the ECG rhythm and disappear with cuff inflation. This probably is not useful in ROSC after cardiac arrest and points 2 or 3 are required.
Start thinking POCUS Blood Pressure
The only useful POCUS pulse is the brachial and it needs to disappear when a manual cuff is inflated – then you know the blood pressure – To be honest – unless you have practiced looking at brachial pulses with ultrasound regularly and recently I don’t know I recommend this one – If this was thought to be a useful end-point then we would need to practice it – I don’t have enough experience with this (in a resus setting) as I haven’t had the opportunity since I thought of it but it isn’t that hard in well patients – Is pulsation enough or should colour doppler be the only endpoint we accept? I don’t know. All sorts of things go wrong in this area. I think pulsation is fair and accommodates all skill levels probably…..
SpO2 Blood Pressure
Occasionally the SpO2 probe on the finger maintains an excellent trace despite horrible blood pressures (<35/- is my most impressive example to date) – In this setting, you can inflate the manual cuff and note when it disappears to measure the BP 4. In the absence of 1, 2 or 3, you best hope you get an arterial line in efficiently because you are in no man’s land –
Repeatedly we see prolonged efforts at placing an arterial line only to find the pressure disastrously low once it is transduced. –
Central vs. Peripheral Arterial Lines
Treatment
I think escalating boluses/infusions of adrenaline/noradrenaline/vasopressin +/- fluids or blood depending on the circumstances. Basically, I have no idea what the right thing to do is and I suspect it depends on the case, likely aetiology and experience (which is a frighteningly unreliable approach). 1, 2 and 3 are the EtCO2 of the circulation as I see it. The measures you can’t argue with. If you don’t have them – you have a problem and there is no point denying it. They are the hard end-points that are needed to avoid loss of situational awareness and the passage of time trying to place arterial lines. Anyway, that is lengthy. Hopefully I’m not saying something really stupid. I think that very few ED’s and ICU’s work as well as yours. I have worked at most hospitals in Melbourne including an ICU fellowship at the Alfred. Very few clinicians have exposure to enough of these patients to be super slick with them – it requires a whole system to work (which is the point of your ED ICU’s but you’re a super specialised crew currently…..). Relying on speed to femoral arterial line placement doesn’t seem robust enough to me. Happy to discuss if it is of any use. I’m truly passionate about this problem as I feel the young lady that died deserves some system change. The yellow zone is a nightmare without an arterial line……
Now on to the Podcast…