Here are links to the three Canadian Paediatric Society’s position statements on Autism:
- Early Detection for Autism Spectrum Disorder in Young Children
- Standards of diagnostic assessment for autism spectrum disorder
- Post-diagnostic management and follow-up care for autism spectrum disorder
In this post, I link to and excerpt from The Canadian Paediatric Society‘s Post-diagnostic management and follow-up care for autism spectrum disorder . Paediatr Child Health 2019 24(7):461–468.
All that follows is from the above resource.
Abstract
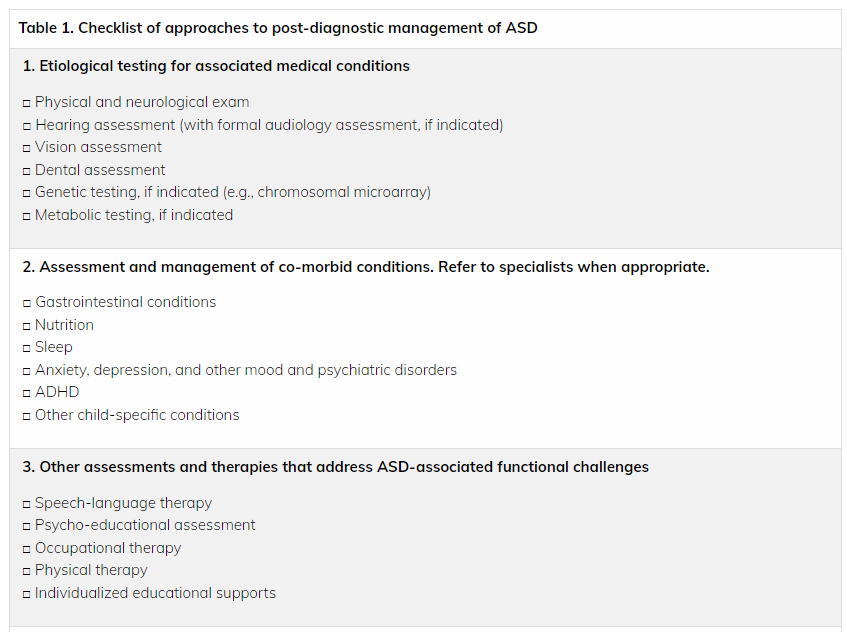
Paediatricians and other primary care providers are well positioned to provide or coordinate ongoing medical and psychosocial care and support services for children with autism spectrum disorder (ASD). This statement provides recommendations and information on a range of interventions and resources, to help paediatric care providers optimize care for children with ASD and support their families. The management of ASD includes treating medical and psychiatric co-morbidities, behavioural and developmental interventions, and providing supportive social care services to enhance quality of life for affected children and families.
Keywords: Autism spectrum disorder; Behavioural interventions; Complementary and alternative medicine; Developmental interventions; Pharmacological management
GENERAL PRINCIPLES AND GOALS OF CARE
Children with autism spectrum disorder (ASD) require individualized medical, behavioural and developmental interventions, and support from social care services, to maximize their full potential.
The overall goals of treatment are to target the core features of ASD, along with associated developmental, behavioural, and learning challenges, and enhance quality of life for the entire family. Specific treatment goals include improving social functioning, play, verbal and nonverbal communication, and functional adaptive skills, as well as reducing maladaptive behaviours, and promoting learning and cognition [1]–[6].
*chromosomal microarray from Mayo Clinic Laboratories.
USEFUL FOR
First-tier, postnatal testing for individuals with multiple anomalies that are not specific to well-delineated genetic syndromes, apparently nonsyndromic developmental delay or intellectual disability, or autism spectrum disorders as recommended by the American College of Medical Genetics and Genomics
Follow-up testing for individuals with unexplained developmental delay or intellectual disability, autism spectrum disorders, or congenital anomalies with a previously normal conventional chromosome study
Determining the size, precise breakpoints, gene content, and any unappreciated complexity of abnormalities detected by other methods such as conventional chromosome and fluorescence in situ hybridization studies
Anxiety
Up to one-half of children with ASD also experience an anxiety disorder or phobia, conditions which may contribute to aggressive or self-injurious behaviours [7][10]. Children with ASD who are verbal, and whose cognitive abilities are at an 8-year-old’s level or greater, may benefit from group or individual cognitive behavioural therapy (CBT) sessions [7][10]. Modified CBT approaches may be appropriate for some younger children.
Attention-deficit hyperactivity disorder (ADHD)
In 30% to 53% of children with ASD, ADHD is a co-occurring condition. Many young children with ADHD are overtly inattentive, hyperactive, or impulsive. With or without ADHD, ‘bolting’ (suddenly running away from caregivers), and wandering in children with ASD, can pose further safety concerns [10]. For more on co-morbid ADHD, see the CPS position statement ADHD in children and youth: Part 3; Assessment and treatment with co-morbid ASD, ID or prematurity.
Depression
If depression co-occurs with ASD, it is generally in older children as they become more socially aware. Children with ASD may be bullied or find it difficult to fit in socially or to establish and maintain relationships [7][10]. Counselling with anticipatory guidance, including referral to community support services or referring a child for psychological intervention, can be helpful.
BEHAVIOURAL AND DEVELOPMENTAL INTERVENTIONS FOR ASD
One constant guiding principle is that behavioural interventions for children with or at risk for ASD should be initiated as early as possible, ideally even before a diagnosis is confirmed [11][12].
Behavioural interventions have emerged as the main evidence-based treatment for children with ASD. These interventions are mostly based on the science of applied behaviour analysis (ABA)* and use systematic learning principles to teach skills in different learning environments [13][15]–[18]. Current evidence supports the integration of ABA-based models with approaches that are informed by developmental theory, particularly with very young children [4][19].
*applied behaviour analysis from raisingchildren.net.au – the Australian parenting website. raisingchildren.net.au has extensive resources on autism that can be helpful for all parents.
MANAGING MALADAPTIVE BEHAVIOURS
Community paediatricians and physicians are often the first-line for helping families manage challenging behaviour, such as aggression or self-injury [4][7]. A trained behaviour specialist can be consulted to help identify reasons for disruptive behaviours (usually based on a functional behaviour assessment*), which then inform first-line treatment planning. Treatment plans may include specific behavioural interventions, an evidence-based parent training program, and environmental modifications, or a combination of approaches. Disruptive behaviours that are pervasive, severe, or interfere substantively with a child’s learning, socialization, health or safety, or the quality of family life, may require using medication concurrently with nonpharmacologic interventions.
*FUNCTIONAL BEHAVIORAL ASSESSMENT (FBA) from New Mexico Public Education Department Technical Assistance Manual.
PHARMACOLOGICAL MANAGEMENT
Co-occurring behavioural symptoms and mental health disorders are common in children with ASD. In most cases, medication use should only be considered when nonpharmacological strategies have been exhausted, and they should always be used in combination with behavioural interventions for children with ASD. Sometimes, starting a medication while awaiting access to services may be necessary, but such decisions must be considered carefully on a case-by-case basis. Because children with ASD can experience more medication side effects than those without ASD, dosing should “start low (often lower than published recommendations), and go slow”. Strict monitoring for adverse effects and drug interactions is essential [28]–[31].
A comprehensive review of pharmacological options for managing challenging behaviours and mental health disorders is beyond the scope of this statement. However, a brief summary of some psycho-pharmacological medications currently in use is provided below, with recommended resources. Physicians are encouraged to review current guidelines when prescribing and monitoring psychotropic medications [28]–[31]. For complex cases, a child psychiatrist or developmental paediatrician should be consulted.
Challenging behaviours
For treating irritability and aggression in children with ASD who are 5 years of age and older, the Food and Drug Administration (FDA) in the USA has only approved two medications: risperidone and aripiprazole. Close monitoring for adverse effects, including weight gain, metabolic syndrome, extrapyramidal symptoms (e.g., muscle stiffness, tremors), and drowsiness is required [30]. Please also refer to the resources below.
Associated behavioural and mental health disorders
Anxiety
Debilitating anxiety can be treated with a cautious trial of a selective serotonin reuptake inhibitor (SSRI), such as fluoxetine or sertraline. Treatment-resistant children should be referred to a tertiary-care specialist [28][29][31].
ADHD
First-line treatment is with methylphenidate or another stimulant medication. Atomoxetine and alpha-2 adrenergic receptor agonists (e.g., clonidine or long-acting guanfacine) are appropriate alternatives, when combined with parent training in ADHD behavioural management [28][29][31].
Depression
Antidepressants, typically SSRIs, may be considered if depressive symptoms persist despite psychosocial interventions [28].
Sleep disturbances
Melatonin, when combined with appropriate sleep hygiene and behavioural modification strategies, appears to be effective in reducing sleep onset times and increasing sleep duration, but may not reduce nocturnal or early waking [2][32]. Side effects may include difficulty waking, daytime sleepiness, or enuresis.
Recommended resources for pharmacological management of ASD
- Canadian Alliance for Monitoring Effectiveness and Safety of Antipsychotics in Children (CAMESA) guidelines: http://camesaguideline.org/information-for-doctors.
- Canadian ADHD Resource Alliance (CADDRA) provides ADHD practice guidelines for physicians: https://www.caddra.ca/.
- American Academy of Child and Adolescent Pscyhiatry (AACDAP) Autism Parents’ Medication Guide: https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/autism/Autism_Spectrum_Disorder_Parents_Medication_Guide.pdf.
Other resources for health care professionals and families:
- Autism Canada. Autism Physician Handbook, Canadian Edition. https://autismcanada.org/resources/physician-handbook/
- Tool kits from Autism Speaks, including tool kits on dental care, feeding, challenging behaviours, and sleep: https://www.autismspeaks.org/tool-kit
- Spectrum: A source for news and analysis of research advances. Individuals can be on a mailing list for updates: https://www.spectrumnews.org/