In this post, I link to and excerpt from The Curbsiders‘ #327 Acute Pancreatitis,
APRIL 4, 2022 By MATTHEW WATTO, MD.
All that follows is from the above resource.
Rapidly treating Acute Pancreatitis might change its course! Learn what you really need to diagnose pancreatitis, when to use imaging sources and what is most important in management! We’re joining Dr. Kaveh Sharzehi @sharzehi of Oregon Health & Science University (@OHSUNews).
Show Segments
- Intro, disclaimer, guest bio
- Guest one-liner
- Case from Kashlak
- Risk factors for severe course
- Use of Scoring Systems
- Requirements to make the diagnosis
- Rational use of imaging
- Initial management: fluids, analgesia, and nutrition
- When to use antibiotics
- When to perform cholecystectomy
- Most common complications and interventions
- How to follow up in the outpatient setting
Acute Pancreatitis Pearls
- Acute Pancreatitis is more severe in patients with higher BMI or Metabolic Syndrome.
- Patients with comorbidities are at high risk for organ dysfunction and we should have a lower threshold for sending them to the ICU.
- Early resuscitation is key to prevent necrotizing pancreatitis.
- CT scan is not needed at time of admission and may be more useful after 72 hours to assess complications.
- It is important to investigate the etiology of pancreatitis because it might change initial management.
- Prolonged bowel rest is not recommended. Early enteral nutrition prevents bacterial translocation and reduces infection.
- Fever and leukocytosis at an early stage doesn’t mandate empiric antibiotic use, as acute pancreatitis alone does not warrant prophylactic antibiotics. Antibiotics may be useful for alternative known infections (i.e. cholangitis, aspiration pneumonia, etc.)
- During transition of care, the provider needs to consider complications of long term endocrine and exocrine dysfunctions.
Acute Pancreatitis Show Notes
How To Diagnose
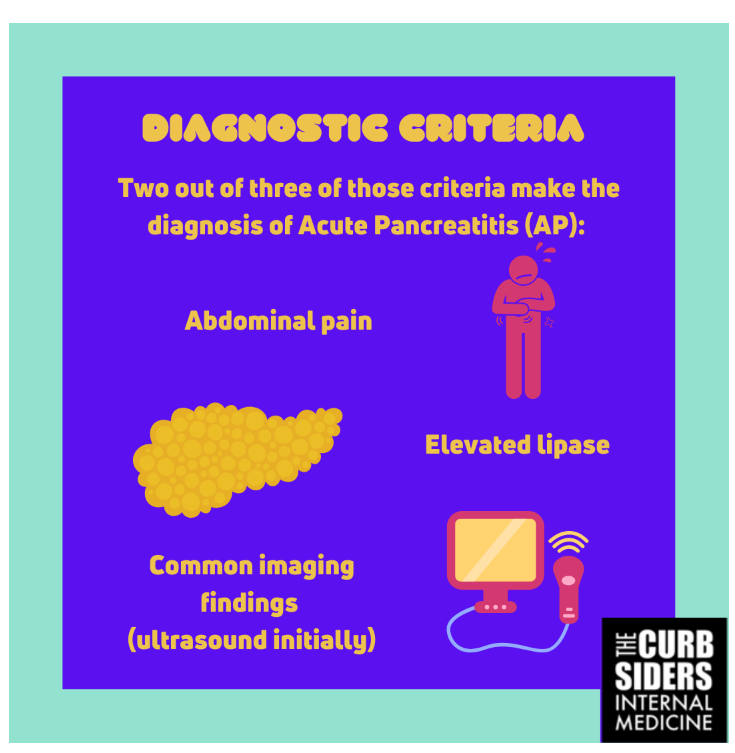
The diagnosis of acute pancreatitis (AP) requires two out of three of the following diagnostic criteria: (1) characteristic abdominal pain (acute, persistent, and severe epigastric pain that can radiate to the back); (2) serum pancreatic enzymes (lipase or amylase) greater than three times the upper limit of normal (ULN); (3) common AP findings on imaging – computed tomography (CT) scan, magnetic resonance imaging (MRI) or transabdominal ultrasound (Banks 2013).
Although elevation of serum pancreatic enzymes is a component of the diagnostic criteria, lipase level does not indicate severity of disease (Lankisch 1999, Holmes 2011). Also, improvement of the value does not correspond to an improvement of clinical condition, as taught by Dr. Sharzehi.
It is Dr. Sharzehi’s expert opinion that cross-section imaging/CT scan within the first 48 hours has very limited value on patient management. It might help if symptomatology or pancreatic enzymes are equivocal, and you need the third item to help make the diagnosis (Boxhoorn 2020). Delayed presentation can cause the serum amylase and lipase to present below three times ULN, requiring imaging to confirm the diagnosis (Banks 2013)*.
*Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Gut. 2013 Jan;62(1):102-11. doi: 10.1136/gutjnl-2012-302779. Epub 2012 Oct 25.
Although some literature endorses contrast enhanced CT scan as the standard for establishing severity, it might not be the best early resource, since it best evaluates peri-pancreatic inflammation and pancreatic necrosis, which tends be detectable 72-96 hours after beginning of the symptoms (Boxhoorn 2020; Chatila 2019; Leppaniemi 2019).
Start here.