In this post, I link to and excerpt from The Curbsiders‘ [Link is to the full episode list] #329 Curing Hepatitis C With Dr. Christian Ramers.
APRIL 18, 2022. By DR EMI OKAMOTO.
Let’s deLiver on the promise of hepatitis C elimination! Dr. Christian Ramers @cramersmd brings hepatitis C diagnosis, care, and cure into the primary care clinic with a simplified algorithm for workup and treatment.
Hepatitis C Pearls
- Baby boomers (born between 1945-1965) were the original target population for hepatitis C screening, because tattoo parlors were non-sterile before the 1990s, blood banks did not screen for hepatitis C, and sexual risk factors. Nowadays all adults should be screened at least once.
- Workup of patients with possible or confirmed hepatitis C should include a complete H&P geared toward evaluating exposure to risk factors (IV drug use, non-sterile tattoos, high-risk sexual behaviors) and extent of liver compromise, as well as serology for HIV and hepatitis B, platelet count, complete metabolic panel, and INR. Consider an abdominal ultrasound of the liver. Genotype testing is no longer routine.
- It is fundamental to evaluate the extent of liver fibrosis in hepatitis C patients, as patients with cirrhosis need longer-term monitoring for cirrhosis with involvement of specialists.
- Both first-line drug combinations (g/p and sof/vel) are pangenotypic and have a cure rate of >95%: everyone who can be treated should be treated. Few exceptions exist (eg life expectancy < 6 months). Ongoing IV drug use is not an exception!
- At the end of treatment for hepatitis C, repeat liver function testing and if abnormal, evaluate for coexisting liver disease (eg alcoholic hepatitis, non-alcoholic steatohepatitis)
- Injection drug related issues do not exclude patients from being capable of receiving and benefiting from hepatitis C treatment: these patients are an opportunity for the integration of addiction medicine and hepatitis C treatment with primary care.
CURRENT RECOMMENDATIONS
Hepatitis C virus (HCV) screening is indicated at least once in all persons aged over 18. This is currently recommended by AASLD-IDSA, CDC, and USPSTF (Havens, 2020). The rationale for augmenting the traditional risk factor-based screening is that up to 45% of persons infected with HCV do not recall or report the classic risk factors (Kim, 2019).
As per CDC guidelines (Schillie, 2020) and AASLD/IDSA guidelines (Ghany, 2019) consider routine periodic screening (Dr. Ramers recommends yearly testing) in persons who are at high risk due to behaviors or exposures. This includes:
- Persons who currently inject drugs or share needles and syringes
- Persons who require long-term hemodialysis or other select medical conditions
- Men who have sex with men
- Persons with HIV
Previously, the traditional, risk-factor based screening had focused screening in:
- Persons with HIV
- Persons with injection drug use (independent of how long ago)
- Persons on maintenance hemodialysis
- Persons with persistently abnormal AST or ALT values
- Those who received blood transfusions or organ transplants before 1992
- Health care personnel exposed to needlestick injuries
- Children of HCV infected mothers
Previous recommendations also singled out baby boomers (born between 1945 and 1965) as an important group for screening as this cohort had up to three quarters of chronic HCV infections detected in the US from 1998 to 2008 (Smith, 2012) . This group includes persons exposed to unsanitary tattoo parlors, blood products and organ transplants without proper screening, and sexual risk factors. All of these are important considerations for a complete history of exposures.
Kashlak pearl: Bloodborne pathogens travel in packs! Every patient with confirmed or suspected hepatitis C should also be screened for HIV and hepatitis B.
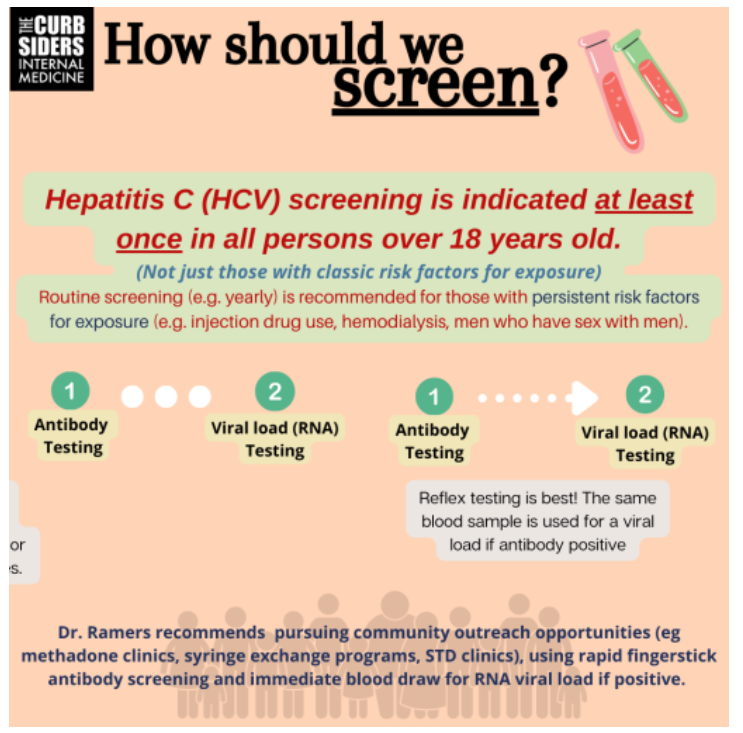
How should we screen?
Traditional 2-step hepatitis C diagnostic processes (antibody testing, then another blood collection for viral load testing) can result in the loss of patients to follow up. Reflex testing (the same blood sample is held for reflex viral load testing if the hepatitis C antibody is positive), is encouraged (Schillie, 2020). Measurement of viral load is performed using FDA-approved nucleic acid tests for detection of HCV RNA copies.
Dr. Ramers recommends pursuing community outreach opportunities for screening (methadone clinics, syringe exchange programs, STD clinics) with fingerstick rapid antibody tests with the resources for immediate blood draws if the hepatitis C antibody is detected so to measure viral load and avoid the loss to follow-up that can occur with two-step testing. A single blood draw with reflex testing is an alternative for community outreach, provided that results are available within a reasonable turnaround time.
Communication with the patient
Language is very important! A positive antibody means that the person was previously exposed to the hepatitis C virus but may or may not have an active infection.. Viral load testing confirms presence of the virus (and active HCV infection) in the patient.
Antibody testing may remain positive for life, though up to 46% of HCV infected persons will spontaneously clear the infection (Seo, 2020), meaning they will have 0 RNA copies. In this scenario, Dr. Ramers recommends emphasizing to the patient that they do not carry any of the virus and are not infected with HCV (there is no latent phase of hepatitis C).
Spontaneous clearance of the virus is associated with female sex, younger age, genetic markers relating to interferon production, and having had acute hepatitis in the course of the disease, with clinical signs such as jaundice or LFT elevations (Lingala, 2015) .
Patient workup
Dr. Ramers recommends all patients with possible or confirmed hepatitis C have a complete history and physical geared towards finding possible exposures to risk factors and the extent of liver compromise (history of cirrhotic complications, stigmata of decompensated cirrhosis).. Also recommended are a platelet count, complete metabolic panel (with LFTs), INR, HIV testing, hepatitis B testing, and pregnancy test when appropriate. Dr. Ramers also considers basic imaging like abdominal ultrasound.
Kashlak pearl: The pretest probability of cirrhosis increases with patient age, thus younger patients with hepatitis C will rarely have advanced liver damage (unless infected since birth). Vigilance for cirrhosis is recommended in older individuals (Gordon, 2015).
Preparing for treatment
Besides the previously mentioned workup, preparation for treatment involves evaluating the degree of liver fibrosis present.
Genotype testing is no longer necessary in most patients diagnosed with hepatitis C, as initial regimens are pangenotypic. The exception to this are patients who are sicker, with cirrhosis, or reinfection. Severe fibrosis is an important consideration as this degree of liver disease is usually related to genotype 3 infection and as such, warrant genotypic investigation, as per AASLD/IDSA guidelines.
Evaluating fibrosis of the liver
Treating hepatitis C infection will stop the progression of hepatitis C-related liver damage. However, you must determine whether any liver damage/fibrosis is present and take measures to prevent further damage from other sources (eg stopping alcohol intake, managing obesity, and controlling steatohepatitis). If cirrhosis is present, management includes screening for hepatocellular carcinoma (Kaplan, 2020). Additionally, those with HCV cirrhosis should be managed by liver specialists or experienced personnel as per AASLD-IDSA guidelines.
Dr. Ramers recommends using a combination of two methods to detect fibrosis: clinical scores and fibrotest. The current paradigm for stratification of liver fibrosis is the METAVIR stage system, which ranges from F0 (no fibrosis) to F4 (cirrhosis).
Commonly used clinical scores are FIB-4 (calculator) and APRI (calculator), both of which use LFT and platelet values. Both of these tests are ‘good at the margins’, for example a FIB-4 score >3.25 is 97% specific for cirrhosis (to rule in) versus <1.45 as 90% negative predictive value for advanced cirrhosis (to rule out), and the values in between are indeterminate.
Various proprietary laboratory fibrosis panels can be used, but are indeterminate at F2 and F3 (intermediate fibrosis). Liver biopsy has fallen out of favor despite being the gold standard, due to being invasive and carrying risks of sampling error and intraobserver variability (Kaplan, 2020).
For situations where clinical scores and/or fibrotest are indeterminate, the definitive test for fibrosis staging is elastography. The cut off values (measured in kPa) for elastography depend on the etiology (or etiologies) of liver fibrosis. There are three elastography techniques: transient elastography (ultrasound-based Fibroscan), acoustic radiation force imaging/point shear-wave elastography (ARFI/pSWE) and magnetic resonance elastography (MRE).
Abdominal ultrasound may not be necessary in all patients, though findings may suggest cirrhosis or discover tumors, nodules, or ascites. Findings that suggest cirrhosis include spleen size > 12cm, portal vein diameter > 12mm, presence of nodularity of liver or coarse echogenicity, and qualitative information about the liver (differences in lobe sizes, shrunken span). Sadly, abdominal ultrasound is insensitive for earlier degrees of fibrosis (Kaplan, 2020).
Kashlak pearl: FIB-4 and APRI depend on LFT values and platelet values, as such, one must consider the existence of other possible conditions that may affect these values; while low platelets may reflect cirrhosis, a splenectomy or relative thrombocytosis as an acute phase reactant may mask this.
Treating Hepatitis C
Drug regimens
This episode covers treatment for straightforward hepatitis C infection; the AASLD-IDSA guideline refers to this as simplified treatment (AASLD/IDSA simplified treatment, without cirrhosis).
For patients with cirrhosis, there is another simplified treatment model which is aimed at patients with compensated cirrhosis (AASLD/IDSA simplified treatment, with compensated cirrhosis).
These simplified algorithms are not recommended for those who have previously been treated for hepatitis C, have cirrhosis, have HIV or hepatitis B, are pregnant, have hepatocellular carcinoma, or have received a liver transplant. These groups are best evaluated by an ID or liver specialist.
There are two initial drug regimens available. They are considered equivalent and shared decision making should guide treatment, weight the length and characteristics of each regimen. Other factors that can determine drug choice are insurance and local availability.
Glecaprevir (300 mg)/pibrentasvir (120 mg) (or g/p) consists of a protease inhibitor (-previr) and an NS5a inhibitor (-asvir). This drug combination is to be taken with food and consists of 3 pills once a day for 8 weeks.
Sofosbuvir (400 mg)/velpatasvir (100 mg) (or sof/vel) consists of an NS5b inhibitor (-buvir) and an NS5a inhibitor (-asvir). This drug combination is to be taken with no particular relation to meals, once a day, for 12 weeks.
An important resource for properly evaluating potential drug-drug interactions is the University of Liverpool Hepatitis drug interaction checker. An important consideration is drugs that suppress gastric acids like antacids and drugs affecting or affected by CYP450, including statins, antiepileptics, and rifampin.
Why do we want to treat everyone?
Treatment will stop the progression of liver damage and its complications.
Treatment can halt transmission of the virus. Even considering people at risk of reinfection, such as injection drug users, models show a reduction in overall prevalence and transmission, suggesting the possibility of a 90% reduction in incidence by 2030 as more people who use injection drugs are treated (Zelenev, 2018).
Follow up
As per the AASLD/IDSA simplified guidelines, no treatment monitoring is necessary in the simplified treatment algorithm of the patient without cirrhosis.
Adverse effects to both first-line therapies include fatigue, headache, and nausea which is often transient and rarely results in discontinuation (Gane, 2019).
The ¨C¨ word (CURE!), is applied when a sustained virological remission is confirmed via viral load testing at 12 weeks (SVR12) following the last day treatment. Both drug regimens have a >95% cure rate, as demonstrated by trials such as ENDURANCE 1 (99% SVR12 with g/p) and ASTRAL 1 (99% SVR12 with sof/vel). If the HCV remains detectable, refer to a specialist as per AASLD/IDSA guidelines.
Kashlak pearl: If liver damage markers such as elevated ALT or AST persist after completing treatment, consider potential other causes of liver damage (alcohol, fatty liver, etc).
Opportunities for integration of care
Injection drug users
Caring for patients with opiate use disorder represents an opportunity for the integration of addiction medicine and hepatitis C treatment into primary care. The SIMPLIFY trial studied people who inject drugs and their adherence to HCV treatment. The study found that treatment can be successful regardless of current injection drug use. Adherence is important though cure rates were relatively high with nonadherence (defined as <90% adherence) (Cunningham, 2018). A conclusion of this study is to prioritize persons who inject drugs for treatment, as this group represents a large amount of new hepatitis C infections around the world and treatment is a means to cut HCV transmission due to needle or syringe sharing (Grebely, 2018). Reinfection rates are low–around 5 per 100 person-years (Hajarizadeh 2020).
Remember to check out other Curbsiders content on the fascinating world of addiction medicine.
Hepatitis C and the primary care provider
¨Shout out to you younger physicians, if you learn (hepatitis C treatment) during your residency, you will be able to do it. (…) Going forward, this should be something all primary care physicians should do¨
- Dr. Christian Ramers
With adequate support, many providers including primary care physicians and advanced practice practitioners can provide successful HCV treatment with appropriate cure rates (Rojas, 2020). Dr. Ramers recommends referral to ID or GI specialists in difficult cases. The Project ECHO course (available for those in New Mexico and/or Indian Country) is another model of training and support.
Dr. Ramers also highlights how positive the experience can be as a provider treating a curable disease! There are significant benefits to the patient when they can cross hepatitis C off their list of problems and often change their lives for the better.
Dr. Ramers recommends the resource State of Medicaid Access for Hepatitis C for readers seeking information on the legal and insurance-related know-how for treatment between states. Some restrictions exist among type of provider, fibrosis level, and sobriety requirements.
Links
- Mountains Beyond Mountains: the Quest of Dr. Paul Farmer, a Man Who Would Cure the World (novel) by Tracy Kidder
- HCV Guidance by AASLD/IDSA: hcvguidelines.org, including for simplified treatment without cirrhosis and with compensated cirrhosis
- State requirements for Medicaid access- StateofHepC.org
- Hepatitis C Online, University of Washington curriculum: www.hepatitisc.uw.edu
- University of Liverpool Hep Drug Interactions Calculator: hep-druginteractions.org
- Project ECHO course (available in select regions)