In addition to today’s resource, please see Resources On Imaging Multiple Sclerosis From Radiopaedia
Posted on July 17, 2022 by Tom Wade MD
Today’s post links to an awesome resource on Multiple Sclerosis for primary care physicians.
The early diagnosis of Multiple Sclerosis matters for primary care physicians because the early diagnosis of MS allows early initiation of disease modifying therapy.
In this post, I link to and excerpt from the Curbsiders‘ [TOC] #344 Multiple Sclerosis with Dr. Annette Okai. JULY 11, 2022 By DEB GORTH.
All that follows is from the above awesome resource.
Transcript-The-Curbsiders-344-MultipleSclerosis.docx
Recognize multiple sclerosis in the clinic, learn how to diagnose it, and partner with your neurology colleagues to help care for these patients. Dr. Annette Okai expertly walks us through multiple sclerosis (North Texas Institute of Neurology & Headache).
Multiple Sclerosis Pearls
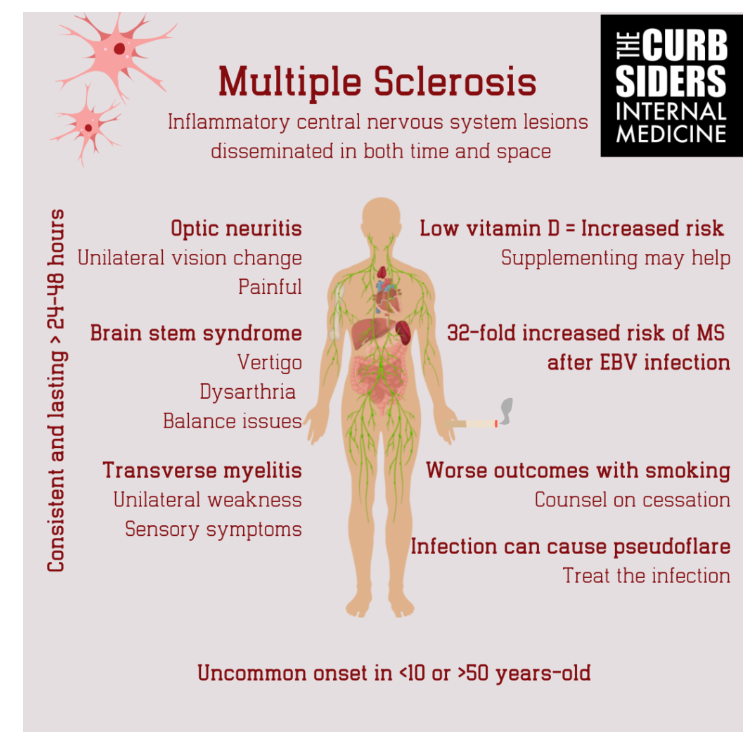
- Multiple sclerosis (MS) typically presents in young adults with a mean age of onset of 20-30 years-old; it is uncommon in individuals less than 10-years-old and greater than 50-years-old.
- Optic neuritis is a common presenting symptom of MS. [The speaker states it is the presenting complaint in 40-70% of cases.]
- Optic neuritis vision changes occur predominantly in one eye and are often painful.
- Symptom persistence is key to diagnosing MS; they should be consistent and last at least 24-48 hours.
- MRI with contrast is the gold standard for imaging MS.
- Current and former smokers have worse MS outcomes.
- In the last thirty years, we have gone from zero approved medications for MS to 23 disease modifying therapies (DMT).
- While DMT for therapies should be managed by a specialist, the PCP can help by managing some of the symptoms of MS.
- Infection can cause a “pseudo flare.” Treat the infection and the symptoms will resolve.
Definitions
Multiple sclerosis is a chronic and progressive autoimmune condition which results in demyelination of the central nervous system. Based on the 2017 McDonald criteria, MS is defined by lesions that must be disseminated in both space (DIS)–at least two different central nervous system sites–and time (DIT)–two different events separated by at least 1 month. The dissemination in time criteria can also be satisfied by the simultaneous presence of both gadolinium-enhancing and nonenhancing lesions at any time on MRI, a new lesion on a follow-up MRI compared to a baseline scan, or oligoclonal bands in the cerebral spinal fluid (van der Vuurst de Vries et al. 2018).
The first appearance of MS disease is called clinically isolated syndrome (CIS). After a second attack occurs and resolves, the disease is now defined as relapsing-remitting MS (RRMS), a phase of MS characterized by bouts of relapse with periods of remission and recovery. As the disease progresses, and the periods of remission wane, the disease now has worsened to secondary progressive MS (SPMS). There is another small portion of patients who suffer from continuous progressive clinical disability without remission called primary progressive MS (PPMS) (Müller et al 2020). The 2017 McDonald criteria allow for MS to be diagnosed during the CIS phase with the presense of oligoclonal bands, which can lead to earlier initiation of disease modifying therapies (Schwenkenbecher et al. 2019).
Etiology
start here