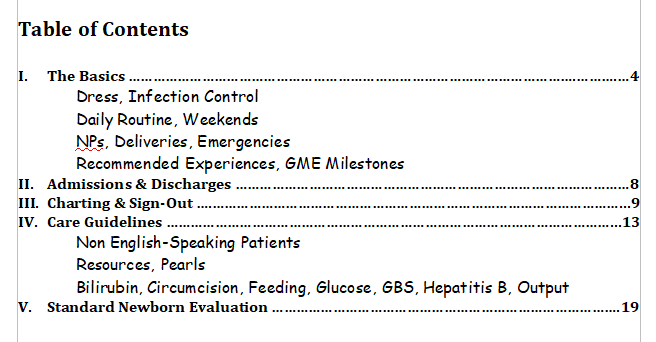
This post contains The Standard Newborn Evaluation template or checklist from The Newborn Nursery Orientation Manual Updated 2014* from the University of Viriginia Children’s Hospital.
*This link downloads the entire manual to your computer. The manual is an excellent newborn memory aid. I’ve included the Table of Contents:
-
Standard Newborn Evaluation
History
1. Date, time and location of birth, referring MD/hospital
2. Birth weight
3. Sex, race
4. Gestational age (EGA)
-
by dates (mother’s estimate)
-
by pre-natal exam (obstetrician’s estimate) (i.e. serial fundal heights, first fetal heart tone, sonography)
-
by post-natal exam – Ballard assessment (estimate)
5. Mother’s age and history of previous pregnancies (Gravid = # pregnancies; Para = # births; AB = # abortions,
spontaneous or therapeutic; living = # children living – summarized, for example, as G3, P2, AB1, L2)
6. Blood types of mother and baby, Coombs test, mother’s antibody screen; ABO & Rh incompatibility
7. Maternal Labs
-
VDRL
-
Hepatitis B
-
HIV
-
GC, chlamydia
-
Group B strep status
-
Amniocentesis-genetic or for lung maturity
8. Complications of pregnancy, labor and delivery
-
Maternal illness/infections
-
Use of drugs, prescribed and non-prescribed
-
Alcohol and smoking
-
Duration of labor/premature labor – tocolytic drugs
-
Duration of rupture of membranes – evidence of maternal infection/colonization culture results/ antibiotic therapy
-
Type of delivery – spontaneous vaginal (SIVA), forceps, C-section
-
Characteristics of amniotic fluid – oligohydramnios, polyhydramnios, meconium stained
-
Abnormal presentation
-
Fetal monitoring
-
Anesthesia used
9. APGAR scores at one and five minutes and every five minutes thereafter until score exceeds six
10. Neonatal course to date
11. Social history
-
Where mother lives
-
Role of father in family
-
Other members of the household
-
Financial support
-
Emotional support
12. Plans for feeding – breast or bottle
13. Plans for well child care and immunizations
Physical Exam
1. Vital signs, measurements
(descriptive terms: T, P, R, BP; Wt, length, head circumference, including percentiles)
2. General appearance
-
level of activity (active/lethargic)
-
general perfusion and color (pink/blue/mottled/pale/yellow; edematous/dehydrated; well developed)
-
nutritional status/state of hydration
-
gross abnormalities
3. Skin
-
vernix
-
capillary hemangiomas (benign): most common on eyelids, forehead, back of neck –
occasionally on trunk or extremities -
mongolian spots (benign)
-
cafe-au-lait spots: > 5 suggestive of neurofibromatosis (if all > 1.5 cm in diameter)
-
milia: superficial epidermal inclusion cysts – generally on face
-
erythema toxicum
-
“parchment skin”: seen in post-term babies
-
dryness, turgor: assess hydration
-
petechiae
-
common, benign: usually on face and upper body – occurs 2° intra-thoracic pressure as the chest passes through the birth canal
-
uncommon: pathologic as a result of thrombocytopenia; important to note distribution and watch for progression
-
-
“sucking blisters”: hands
-
abrasions
-
peeling of skin in postmature baby
-
jaundice
4. Head
-
shape
-
molding
-
asymmetry: may be normal 2° fetal posture or abnormal 2° structural defect
-
appearance
-
bruising
-
scalp: internal monitor sites, scalp blood sampling sites
-
forceps marks
-
hair distribution
-
palpation
-
caput succedaneum: diffuse, generally symmetric scalp edema 2° vertex presentation (usually resolves in first few days); edema crosses sutures
-
cephalohematoma: sub-periosteal hemorrhage; feels like boggy edema but is located over one particular bony area; may take months to resolve; never crosses sutures; can indicate linear skull fracture or more occult intracranial bleeding
-
sutures: craniotabes is a soft area in parietal bone near the sagittal suture
-
palpable fractures
5. Fontanelles
-
anterior and posterior
-
may suggest increased intracranial pressure if bulging open wide fontanelle extending into frontal area
6. Eyes
-
may be hard to assess in first 24 hours due to edema of lids
-
reactiveness of pupils (PERRL = Pupils equal, round, reactive to light)
-
red reflex exam for retinoblastoma, corneal opacities
-
lens
-
test for congenital cataracts
-
discharge
-
conjunctival hemorrhage: common, may be benign; occurs 2° increase in intra-thoracic pressure when the chest passes through the birth canal
-
inter-canthal distance: if increased or decreased may suggest a congenital syndrome
7. Ears
-
external appearance: shape and position
-
low set ears may suggest a congenital syndrome such as Down syndrome
-
-
external canals: check for patency, atresia
-
tympanic membranes: canals may be too tortuous to allow visualization
-
preauricular sinus and tags: may be associated with renal anomalies/hearing loss
8. Nose
-
external appearance: congenital abnormalities, atresia
-
flaring of nostrils: may suggest respiratory distress
-
patency of nares: congestion/discharge
9. Mouth
-
external appearance: cleft lip, shape, etc
-
precocious dentition (supernumerary teeth)
10. Palate
-
structural abnormalities
-
cleft: may lead to feeding problems aspiration etc. in the immediate neonatal period
-
high arched: may suggest congenital syndrome
-
lesions
-
Epstein Pearls: whitish nodules on palate; benign, common; accumulation of epithelial cells
-
11. Neck
-
tone: increased may indicate neurological disease
-
palpitation: masses include thyroid, cystic hygroma, branchial cleft/cysts
-
mobility: congenital torticollis (may palpate mass as well)
12. Chest
-
appearance
-
-
congenital deformities may cause asymmetry
-
retractions: sub-xiphoid or intercostal suggest respiratory distress with increased effort of breathing
-
-
respiratory pattern: rate and rhythm commonly quite variable; > 60 resp/min for sustained time is abnormal
13. Lungs
-
auscultation
-
-
rales, wheezes, rhonchi, grunting
-
compare air movement on each side and between lung zones
-
14. Heart
-
cyanosis: central vs acrocyanosis
-
precordial activity
-
rhythm and rate (RRR = regular rate and rhythm)
-
commonly quite variable
-
may range from 100-180 in various states of rest/activity
-
extra systoles and sinus pauses common
-
S1, S2: may be grossly abnormal in valvular heart disease
-
murmurs
-
-
murmur = m
-
grade I-VI (written e.g. II/VI)
-
describe location and quality
-
murmurs in first day from a closing ductus are common
-
any murmur still present on third day should be evaluated
-
-
gallops
-
extra heart sounds very difficult to hear at the rapid heart rate of a newborn
15. Pulses
-
palpate in each extremity and compare side to side and UE to LE
-
decrease in LE pulse or delay in transmission to LE vs UE may indicate coarctation of the aorta
-
pulse graded 0-4+: 0 = Absent, 2+ = Normal, 4+ = Bounding
16. Abdomen
-
observation: distended, discolored, scaphoid
-
bowel sounds: may not be present early in life
-
palpation: for masses, distension etc.
-
umbilicus: number of cord vessels
-
liver: commonly palpable up to 1 cm below the right costal margin
-
spleen: may be just palpable under left costal margin
-
kidneys: usually palpable, at least in part, in a very relaxed infant who allows deep palpation; palpable large kidneys suggestive of hydronephrosis
17. Genitalia
-
inspection
-
-
examine all structures to ascertain if they are clearly male or female
-
particularly check for location of the urethral orifice; may be displaced (hypospadias, epispadias) in what appears to be male infant (may be male or virilized female)
-
foreskin is often tight and appears closed
-
female genitalia may appear enlarged in proportion to the other body structures 2° the effects of maternal hormones and/or prematurity
-
-
palpation
-
-
palpate for testes in the scrotum or inguinal canal
-
scrotal enlargement may be 2° hydrocele which is relatively common – diagnose by transillumination as well as palpation (intermittent, recurrent hydrocele is suggestive of hernia)
-
testes may be in canal or not palpable in ELBW infant
-
-
discharge
-
females may have a clear mucous discharge or even blood (“pseudomenses”) 2° hormonal stimulation in utero with sudden withdrawal in post-partum
-
-
circumcision
-
may look quite edematous and erythematous
-
watch for difficulty urinating after procedure
-
18. Breasts: may not be visible in ELBW; term infant may have prominent breast tissue, hormonally stimulated
19. Rectum: check for patency (evidence of stooling), fissures (may see bloody stools), placement (may be
anterior)
20. Hernia: check inguinal regions; diastasis recti (midline weakness of the abdominal musculature) is common
and may simulate a ventral hernia
21. Spine
-
inspect and palpate for deformity, deviation
-
inspect for dermal sinus tracts: may be anywhere along the midline from the nose, over the skull and down the spine to the sacrum
-
any dimple should be carefully examined to be sure that the bottom of the pit is visible (traction on the skin helps exam)
-
any discoloration or hairy lesion should be evaluated
22. Clavicles: inspect for asymmetry; palpate for fractures (common birth trauma)
23. Extremities
-
inspect for deformities – fetal position may cause some apparent abnormalities that are self-correcting
-
check joints or observe for range of motion: term infants are normally quite flexed as a general posture
-
check palmar creases
-
hips – test for congenital dysplasia by:
-
observing for differences in leg movement
-
check for differences in leg length
-
checking for asymmetry of leg skin folds (misleading)
-
manipulation of the hips (abduction) with fingers over the greater trochanter and feeling for (or hearing) clicks
-
Barlow & Ortoloni maneuvers
-
Digits: count them; extra digit buds or skin tags are not uncommon (often familial)
24. Neuro
-
degree of alertness
-
spontaneous movement
-
posture
-
tone
-
grasp, suck, Moro, root
-
DTRs
-
response to light, sound
-
facial, brachial plexus palsies
25. Cord (Umbilicus)
-
check for secure clamping
-
count and document the arteries (2, thick-walled) and vein (single, thin walled) in the remnant
26. Voiding
-
95% of infants void in the first 24 hours
-
98% void in the first 48 hours
-
most common reason for “delay” in voiding is missing urination at birth
27. Stools
-
90% of infants pass stool in the first 24 hours
-
98% stool in the first 48 hours
-
prolonged time without stooling suggests meconium ileus (cystic fibrosis), meconium plug, or other congenital defect