The RUSH Protocol (Rapid Ultrasound In Shock) [Direct Link to Dr. Turner’s YouTube video]
Previously, I have posted Dr. Turner’s teaching videos on the eFAST exam (extended Focused Assessment with Sonography in Trauma) and the FATE exam (Focused Assessment of Thoracic Echocardiography). Today I’m posting her outstanding video on the RUSH protocol (Rapid Ultrasound In Shock) at the end of the notes. And after the video, there are more notes from Dr. Turner’s video. Be sure to watch all the way through as starting at 31:30, Dr. Turner presents three great case studies which brilliantly cover everything in the video–don’t miss it!
All that follows is from Dr. Turner’s video:
The RUSH protocol is used in the evaluation of shock. This ultrasound exam can answer non-invasively the questions that in the past could only be answered with a pulmonary artery catheter.
The pulmonary artery (PA) catheter can be used to:
- Measure Central Venous Pressure (CVP)
- Measure Pulmonary Artery Pressure (PAP)
- Calculate Cardiac Output and Cardiac Index (CO and CI)
- Calculate Systemic Vascular Resistence (SVR)
- To Suggest Other Problems (Cardiac Tamponade, Valvular Stenosis, Valvular Insufficiency)
So the PA catheter can help us determine why the patient is in shock or what is the etiology (mechanism) of the shock. For the patient with respiratory failure the PA catheter can help us determine whether the etiology is cardiogenic or non-cardiogenic pulmonary edema. And we can use the PA catheter to follow the effect of our therapeutic intervensions (that is, what is the effect when we give fluids or pressors). However, the PA catheter is fraught with complications and technical pitfalls and is not much used at present.
Physician performed bedside ultrasonography can answer all the questions that the pulmonary artery catheter can answer. And ultrasound can do it more rapidly, and without any of the risks of a pulmonary artery catheter.
With Bedside Ultrasound we can non-invasively:
- Estimate central venous pressure using inferior vena cava respiratory variation
- Estimate pulmonary artery pressure using the tricuspid regurgitation signal
- Pulmonary capillary wedge pressure can be estimated
- Cardiac output and cardiac index can be calculated
- Systemic vascular resistance can be calculated from the other parameters
- And other problems can be diagnosed (cardiac tamponade, valvular dysfunction, systolic dysfunction)
The RUSH protocol is used to evaluate the critically ill patient in shock. The speaker organizes the exam into three conceptual steps:
- The pump (the heart): LV contractility, RV function (pressure or volume overload or dysfunction), pericardial effusion
- The tank (the volume of fluid in the circulation): Inferior Vena Cava Variation (to estimate fluid status), leaks (as evidenced by the ultrasound detection of thoracic fluid, pericardial fluid, or abdominal fluid), things interfering with the flow of fluid in the tank (tension pneumothorax, pericardial tamponade, abdominal compartment syndrome)
- The pipes: aortic dissection, aortic aneurysm, deep venous thrombosis
The RUSH protocol (Rapid ultrasound in shock) exaluation can also be thought of as HI MAP (and a high mean arterial pressure is what we want for the patient in shock). So we evaluate:
- The heart (using the FATE protocol)
- The inferior vena cava (to assess fluid status and fluid responsiveness)
- Morrison’s pouch (to look for intra-abdominal fluid)
- The aorta and veins
- The pleura (looking for pneumothorax evidenced by the lack of pleural sliding and looking for fluid in the pleural space)
The above is simply another way of looking at the pump, the tank, and the pipes.
The categories of shock include:
- Hypovolemic (less fluid in the tank)
- hemorrhage
- dehydration from GI or renal fluid loss
- Distributive (the tank has gotten larger)
- sepsis
- adrenal insufficiency
- neurogenic shock
- vasoplegic states
- Cardiogenic (the pump can’t perform properly)
- diastolic dysfunction
- systolic dysfunction
- severe valvular dysfunction
- Obstructive (the tank can’t fill the pump)
- hypertrophic obstructive cardiomyopathy with systolic anterior motion of the mitral leaflet
- massive pleural effusion and ascites
- cardiac tamponade
- tension pneumothorax
- pulmonary embolus
Now let’s watch Dr. Turner’s outstanding teaching video.
At about 12:30 in the video Dr. Turner identifies a crticical question that we want to answer in our shocky patients: “Will they be volume responsive?” And what we are asking is: Is our patient on the steep part of the Frank Starling Curve where a fluid challenge will increase cardiac output. And the answer can be yes, even in patients with poor systolic function. So how do we decide?
In the past we would look at static parameters to answer that question:
- CVP
- IVC diameter
- LVEDD
- LVEDA
But the above has not been shown to be predictive of volume responsiveness. Instead, we now focus on dynamic parameters.
Approx 13:20: Increased intrathoracic pressure will decrease venous return (in a spontaneously breathing patient, this will be during exhalation and in a ventilated patient–it will occur during inhalation. Decreased intrathoracic pressure will increase venous return.
The Frank-Starling law predicts that for a change in preload, you will change your stroke volume or cardiac output.
“If when a patient is breathing, it is affecting their stroke volume, then they are on the steep part of the Frank-Starling Curve [that is a volume infusion will increase stroke voume/cardiac output]. How do we tell that?”
13:55: We tell that by dynamic parameters:
- IVC Distensibility Index
- Delta VTI (Velocity Time Integral)
- Delta Vmax
- Passive Leg Raising
- Hyperdynamic “kissing papillary sign”
Dr. Turner clearly explains these signs in video from 14:20 to
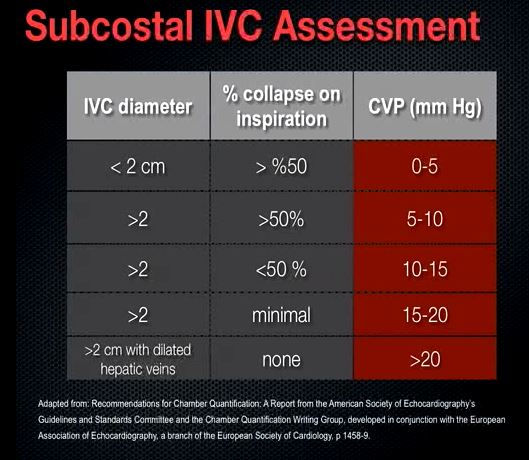
Dr. Turner reminds us that Central Venous Pressure (CVP) does not predict volume responsiveness except at the extremes. “If your central venous pressure is zero to two, then you can pretty much assume that the patient will benefit from volume if they are in shock. And likewise, if the central venous pressure is greater than 20, then the chances that the patient will benefit from volume is low. But in between your guess is as good as mine.” In another video*, Dr. Turner observes that in the intermediate cases other dynamic measures need to be assessed. [Dr. Turner gives more detailed information on estimating IVC pressure in her video *The Fate Exam: Focused Assessed Transthoracic Echo from 5:25 to 9:50. The Subcostal IVC Assessment is from this video.]
 From 16:20 to 17:50, Dr. Turner discusses Delta Vmax and Delta VTI. These are rather advanced concepts in doppler measurement and making these measurements is technically demanding. This discussion simply introduces the terms.
From 16:20 to 17:50, Dr. Turner discusses Delta Vmax and Delta VTI. These are rather advanced concepts in doppler measurement and making these measurements is technically demanding. This discussion simply introduces the terms.
From 17:50 to 18:20, Dr. Turner goes over the IVC Distensibility Index (IVI). The IVC Distensibility Index is: IVC max – IVCmin IVCmean
If the IDI is greater than 12% then the patient will respond to volume. And using the M-mode cursor is a great way to get the numbers.
From 18:20 to 19:05, Dr. Turner discusses the “Kissing Papillary Sign”. When the papillary muscles touch (“kiss”) each other in systole in the apical four chamber or parasternal short axis, “you are obliterating the cavity. And this typically represents hyperdynamic states such as hypovolemia and distributive shock.”
“Passive Leg Raise” is discussed by Dr. Turner from 19:05 to 20:20. This is a means of giving a reversible fluid bolus to see if it increases cardiac output.
“So we’ve assessed whether the tank is full by looking at the heart and the inferior vena cava. We also want to see if there is any leaking going on (the “leaky tank”).”
We assess for a leaky tank with the views of the Focused Assessed Sonography in Trauma (FAST) exam. Dr. Turner very briefly reviews this exam from 20:20 to 22:10. Dr. Turner clearly and completely explains and demonstrates the FAST exam in her YouTube Video, eFAST: extended Focused Assessment with Sonography in Trauma.
22:10 to 24:30: We also need to look at the pipes (arteries and veins) because they can be the cause of shock.
From 24:30 to 31:00, Dr. Turner reviews obstructive shock, “processes that physically impair cardiac output”:
- Pneumothorax
- Pericardial Effusion
- Pulmonary Embolus
- Intra-abdominal Hypertension
- Massive Pleural Effusion
- Hypertrophic Obstructive Cardiomyopathy with Systolic Anterior Motion (HOCM with SAM)
From 31:00 to 31:25 of the video, Dr. Turner summarizes how to think about the RUSH exam in a systematic way. “We want to think about the pump; think about the tank; and think about the pipes.”
Another way we can think about the exam, Dr. Turner states, is HI-MAP. HI MAP is what we want for our patient in shock–we want a high mean arterial pressure for the patient. The mean arterial pressure is equal to the sum of 1/3 of the systolic blood pressure and 2/3 of the diastolic blood pressure. Or equivalently MAP = [2(diastolic pressure) + systolic pressure] / 3
- Heart
- IVC
- Morrison’s Pouch
- Aorta and Veins
- Pleura
In the final part of this video beginning at 31:30, Dr. Turner goes over three excellent teaching cases.




