This post contains links to and excerpts from What is the utility of measuring the serum ammonia level in patients with altered mental status [Full Text HTML] [PubMed Abstract] [Full Text PDF]. Cleve Clin J Med. 2009 Apr;76(4):252-4. doi: 10.3949/ccjm.76a.08072.
Here are the excerpts:
Question:
What is the utility of measuring
the serum ammonia level in patients with altered mental status?Answer:
If you already know that the patient with altered mental status has decompensated liver disease, measuring the arterial or venous ammonia level has little utility. In these patients, one’s clinical suspicion is the main guide to diagnosing hepatic encephalopathy, and a normal or modestly elevated blood ammonia level does not rule out the diagnosis.
On the other hand, provided that it is appropriately performed, blood ammonia testing
may be helpful if there is no clear evidence of
underlying chronic liver disease. In these cases, an elevated blood ammonia level may have significant prognostic value (as in acute liver failure) or may prompt you to initiate further evaluation for uncommon but significant metabolic disorders such as urea cycle disorders.
WHEN AMMONIA LEVELS RISE
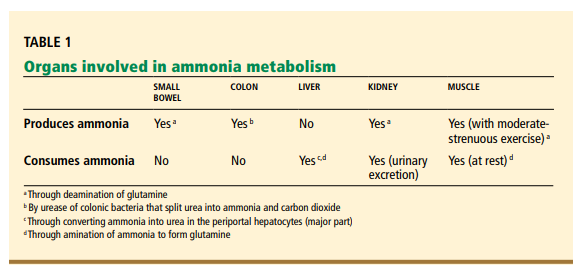
Ammonia is derived predominantly from protein degradation. Most of the ammonia in the
blood comes from the intestine, where colonic bacteria use ureases to break down urea into
ammonia and carbon dioxide.[The liver converts ammonia to urea which is then excreted in the kidneys.]
Ammonia levels are elevated in several
conditions in which its production is increased (eg, in convulsive seizures with increased muscle production) or its clearance is impaired (eg, in hepatocellular dysfunction, portosystemic shunting, or both, with subsequent impaired hepatic detoxification of ammonia).Because the blood-brain barrier is highly
permeable to ammonia, the brain is exposed
to excessive concentrations of it in these circumstances. In the brain, ammonia is thought
to cause both functional and structural abnormalities that could explain neuropsychiatric
dysfunction, often manifested as an altered
mental status of variable degree.1–3If the patient is known to have
chronic liver diseaseIf the patient is known to have chronic liver
disease, we usually do not need to measure the
blood ammonia level because normal levels in
these patients do not rule out hepatic encephalopathy.Altered mental status in cirrhotic patients
does not always equal hepatic encephalopathy. Regardless of the degree of blood ammonia elevation, other relevant causes of altered mental status should be excluded on the basis
of the clinical presentation.Computed tomography of the head is usually obtained in cirrhotic patients:
- Who have changes in mental status but
whose presentation is not typical of hepatic encephalopathy (such as those with
focal neurologic signs);- In cases of severe hepatic encephalopathy, suspected head trauma (especially given the commonly associated coagulopathy in cirrhotic patients), and hepatic
encephalopathy resistant to standard
therapy; and- Without clear precipitating factors for hepatic encephalopathy, such as infection
(eg, spontaneous bacterial peritonitis) and
renal insufficiency.Similarly, in alcoholic patients who present with altered mental status, we should always consider Wernicke encephalopathy