In addition to all of the outstanding resources on Type 2 Diabetes which The Curbsiders have given us [and that I list below], please see my posts:
- Link To CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2020 EXECUTIVE SUMMARY
Posted on November 28, 2020 by Tom Wade MD - Links to The [Complete] Standards of Medicare Care In Diabetes-2020 From the American Diabetes Association
Posted on April 13, 2020 by Tom Wade MD - Links To And Excerpts From “Standards of Medical Care in Diabetes—2020 Abridged for Primary Care Providers”
Posted on April 12, 2020 by Tom Wade MD
In this post I link to and excerpt from #243 Diabetes [Type 2] Triple Distilled, NOVEMBER 23, 2020 By DR MOLLY HEUBLEIN from The Curbsiders.
The Curbsiders write:
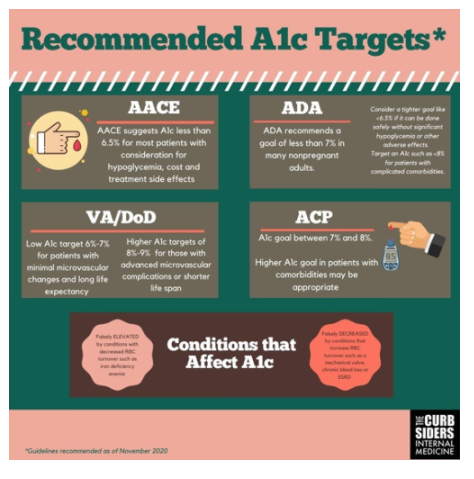
Listen in as we recap four of our favorite diabetes episodes to bring you the pearls you need to stay up to date on type 2 diabetes management in the clinic. We cover pitfalls of A1c testing, guidelines for A1C targets, when and how to use the newer medications SGLT-2 inhibitors and GLP-1 agonists. We wrap up with a discussion of managing DM2 in patients with kidney disease and in which patients to consider de-intensifying treatment. Feel confident managing diabetes with the latest data in 2020!
Here is the podcast:
Curbsiders Episodes Covered:
#51: Diabetes Treatment in 2017 Dr. Jonathan D. Laffert reviews AACE guidelines. Air date: August 7, 2017
#96: Diabetes: A1C targets & ACP guidelines controversy Dr. Devan Kansagara discusses ACP guidance statements with a nice review of original type 2 diabetes trial data. Air date: May 21, 2018
#168 Diabetes Update Dr. Jeff Colburn reviews DOD/VA guidelines and goes into medications in more detail. Air date: August 26, 2019
#204 SGLT-2 Inhibitors NephMadness deep dive into SGLT-2s. Air date: April 6, 2020
Here are excerpts from #243 Diabetes Triple Distilled:
Diabetes Triple Distilled Pearls
- The hemoglobin A1c value can be artificially higher in patients who have conditions that cause prolonged red blood cell survival and artificially lower in patients with higher red blood cell turnover.
- Tight A1c control itself with pharmacotherapy has not reliably shown patient centered benefits- this may be changing with our new medications!
- SGLT-2 inhibitors lower blood sugar without significant hypoglycemia, encourage weight loss, and lower blood pressure. They reduce heart failure complications, slow progression of CKD, reduce CVD, and lower death rates.
- GLP-1 agonists lower blood sugar without significant hypoglycemia and encourage weight loss. They reduce cardiovascular disease outcomes and lower death rates.
- Consider de-intensifying therapy in diabetic patients treated with pharmacotherapy with an A1c <6.5% if they do not have specific indications for SGLT-2 inhibitors or GLP-1 agonists.
MACROVASCULAR/MICROVASCULAR BENEFITS
Studies looking at older medications including sulfonylureas, metformin, insulin, and thiazolidinediones (TZDs) do not consistently show a benefit for macrovascular benefits, with a possible exception of metformin after many years of use. Tighter A1c control reduces surrogate endpoints for microvascular disease such as albuminuria, photocoagulation for diabetic retinopathy and painful peripheral neuropathy (Rodriguez-Gutierrez R 2016).
Newer medications: SGLT-2 Inhibitors and GLP-1 Agonists
BENEFITS OF THESE NEWER MEDICATIONS
The new classes of medications were studied as secondary prevention in patients with underlying CKD or cardiovascular disease and have shown significant benefits in reduction in cardiovascular, renal disease, and even death regardless of A1c targets (Tuttle 2020, Lee 2020)
SGLT-2 INHIBITORS
Sodium glucose cotransporter-2 inhibitors are oral medications cause glucosuria and natriuresis. SGLT-2 inhibitors lower blood sugar by causing loss of glucose in the urine- leading to a low risk of hypoglycemia while having the added benefits of lowering blood pressure and encouraging weight loss. These drugs have been shown to reduce death, cardiovascular disease outcomes, and lower heart failure complications and kidney disease progression (Tuttle 2020). Clinicians should be aware that these drugs pose an increased rate of genital fungal infections (Johnnson 2013), while rates of urinary tract infections are not significantly increased (Sarafidis 2020). Other rare adverse risks include euglycemic diabetic ketoacidosis (DKA) and Fournier’s gangrene. The FDA removed the black box warning for increased risk of amputation, but still reports a small amputation risk with canagliflozin. Watch for hypovolemia and/or hypotension when starting these in patients with tight blood pressure control or on thiazide diuretics (Tuttle 2020).
GLP-1 AGONISTS
Glucagon-like peptide 1 agonists are drugs that improve glucose dependent insulin release from the pancreas, decrease the secretion of glucagon and slow gastric emptying; as such, the most common side effects to discuss with patients include nausea, early satiety and weight loss. These agents have a low risk of hypoglycemia alone, though Dr. Colburn warns of potential hypoglycemia in combination with sulfonylureas or insulin (he suggests reducing 20-30% insulin dose reduction when adding GLP-1 agonists). They are given as a once daily or once weekly injections, or more recently semaglutide is available as once daily oral. Once weekly dosing can take up to 5 weeks to reach steady state drug levels, so blood sugar reduction builds slowly. There is a concern for an increased risk of medullary thyroid cancer in animal studies; best practice is to avoid using these in patients with MEN syndrome or a history of medullary thyroid cancer. The data regarding pancreatic cancer and pancreatitis is inconclusive, there may be an increased risk so probably best to avoid in patients with a history of pancreatitis. GLP-1 agonists have been shown to reduce death and cardiovascular outcomes (Lee 2020, Zheng et al 2018)