Note to myself:
- The Johns Hopkins ABX (Antibiotics) Guide [link is to the Index] is only $30 a year for an online subscription and the resource I have chosen [not affiliate links].
- The Internet Book Of Critical Care [link is to the Table Of Contents], by Dr. Josh Farkas, is an awesome online resource for all topics in critical care including infectious diseases. Here are direct links to all subsections of the Table of Contents. Each of the subsections has entries relevant to Infectious Disease and The IBCC can be used for infectious disease help:
In this post, I link to and excerpt from #284 An Antibiotics Primer, with @IDdocAdi
JULY 12, 2021 By NORA TARANTO by The Curbsiders.
All that follows is from the above podcast and show notes.
Antibiotics Pearls
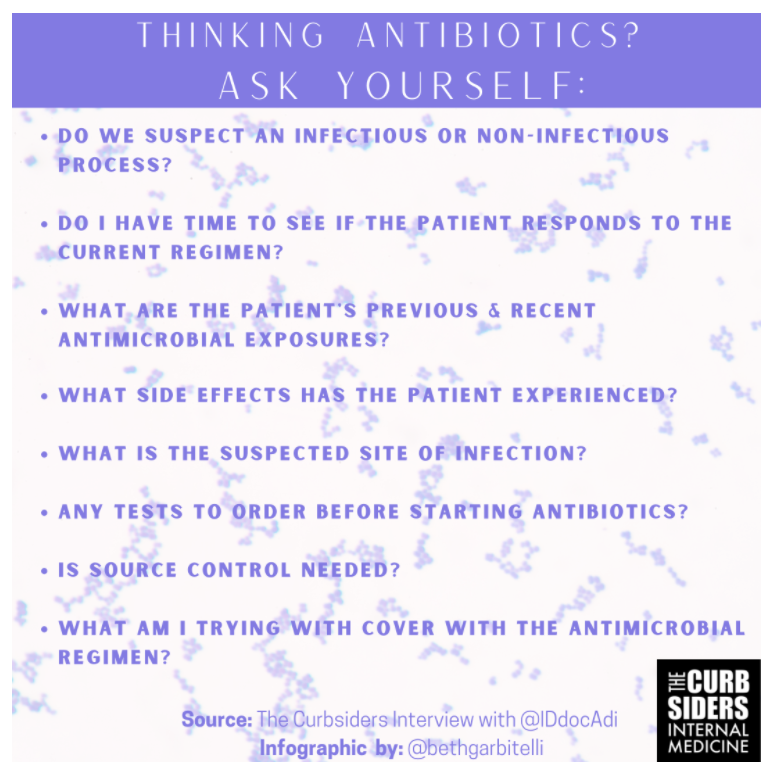
- Use Dr. Shah’s broad questions to guide your cognitive framing of antibiotic use and stewardship (see graphic).
- Antibiotic stewardship is not just about stopping antibiotics. It is about making the right antibiotic choice, at the right dose, for the right duration, for the right patient. Always look at your patient before starting your antibiotic.
- Whether you are treating a patient with advanced dementia or advanced cancer, remember that medications have adverse effects and side effects: Remember this, before empirically treating everyone with Vanc-o-Pime (Vanc and Cefepime).
- Look for the antibiogram at your local institution, to identify drugs that might not be so good to use in your area.
Antibiotics Primer
The Framework
Dr. Shah recommends thinking about why you are choosing a specific antibiotic. He has a few questions he asks himself:
- Do we suspect an infectious process or non-infectious process?
- Do I have time to see if the patient responds to the current regimen, or do I need to cover broadly, immediately? (aka Just how sick is the patient?)
- In deciding on empiric coverage, what are previous antimicrobial exposures, and what side effects has the patient experienced?
- What is the suspected site of infection?
- Any tests to order before starting antibiotics? (Think blood cultures!)
- Is source control needed?
- What am I trying to cover with the antibiotic regimen?
Think critically about the patient’s presentation, per Dr. Shah (e.g. with a swollen extremity for several months, does it make sense to classify that as cellulitis that requires broad spectrum antibiotics?). Don’t be afraid to stop antibiotics.
Some Helpful Tidbits, to Start
Resources, when you don’t know what to pick: A couple of suggestions: Johns Hopkins Antibiotics Guide, Mayo Clinic Antimicrobial Therapy Quick Guide, Sanford Guide, and (as always) UpToDate *
*All of the above have online subscription options.
Dr. Shah’s Favorite Antibiotic: Doxycycline. Works against Cellulitis, Bartonella, Ticks, COPD exacerbations, atypical pneumonia, CAPs, *some STIs, penicillin-resistant syphilis, and Acne. And it’s Oral! What more could you ask for?! He also likes Quinolones (for some situations), and TMP-SMX for others, given both have good oral bioavailability.
Common Antibiotic Pearls and Pitfalls:
- Pip-Tazo covers anaerobes (So no need to empirically add metronidazole)
- Daptomycin does not work for pneumonia (it is sequestered by surfactant) (Silverman 2005).
- You do NOT need metronidazole for aspiration pneumonia coverage, unless you are treating an empyema or lung abscess. (Watto’s advice: please do not use clindamycin for ‘aspiration pneumonia’ either! (ATS 2019)
- When using azithromycin or levofloxacin, check the QT interval.
- Just because patients are in the hospital does not mean they need to be on IV Antibiotics the entire time. Check out Brad Spellburg’s IV to PO comparison charts.
Short Courses!
More evidence is emerging for the efficacy and safety of shorter courses of antibiotics (Lee 2021). You can discontinue abx in community acquired pneumonia after 5 days, as long as you see improvement and clinical stability (Lee 2021). For more best practices, check out the ACP’s June 2021 recommendations on short courses for common infections.
WHO IS AT-RISK FOR MDRO? FOR MRSA?
If patients have been recently exposed to a healthcare setting, if they are on dialysis, or if they are coming from an assisted living/nursing home, you may want broader coverage for drug resistant organisms. If there is a clear abscess on imaging, you should cover for MRSA as well. For more on MRSA risk factors, check out this 2020 StatPearls Article.
WHEN TO DOUBLE-COVER FOR PSEUDOMONAS?
WHEN TO DOUBLE-COVER FOR PSEUDOMONAS?
If you have a patient heavily exposed to health care settings–especially if they have high-risk features such as recent chemotherapy, bone marrow transplant, solid organ transplant, or are in the ICU on several pressors–it is reasonable to use two antipseudomonal agents upfront. Options include pip-tazo + levofloxacin or tobramycin, pip-tazo + amikacin, cefepime + tobramycin or amikacin or levo. But, if stable, double coverage may not be necessary.