In this post I link to and excerpt from
- Rural Medicine Case: Angle Closure Glaucoma
- Helman, A. Long, B. Khatib, N. Strayer, R. Hensley, J. Foohey, S. Petrosoniak, A. EM Quick Hits 36 – Surviving Sepsis, Angle Closure Glaucoma, Bougies, Frostbite, Hot/Altered Patient, Central Cord Syndrome. Emergency Medicine Cases. March 2022. https://emergencymedicinecases.com/em-quick-hits-march-2022/. Accessed 3-7-2022.
- This is the link to the above podcast. 11:59-20:50
- Medical Concepts: Acute Angle Closure Glaucoma
In Medical Concepts by Stephanie Cargnelli October 11, 2016 from CanadiEM
All that follows is from Rural Medicine Case: Angle Closure Glaucoma from EM Quick Hits 36
Background
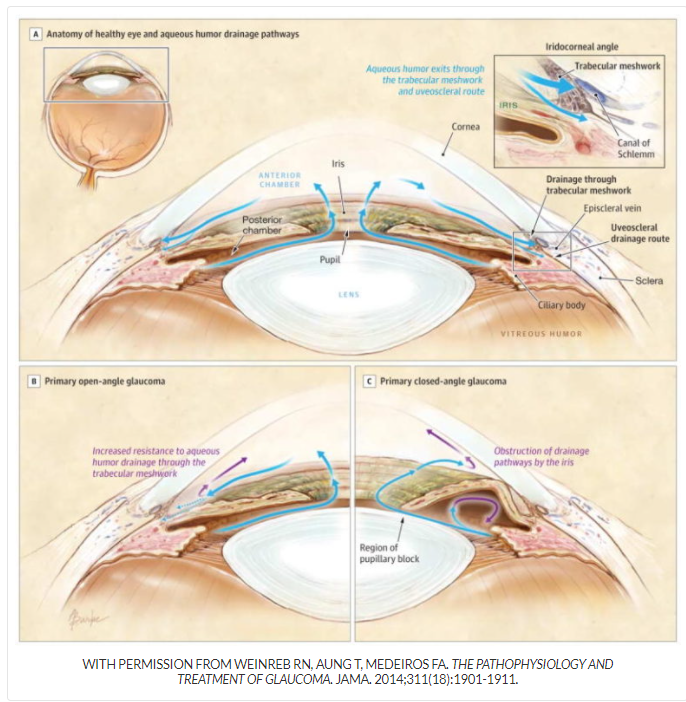
- Raised intra-ocular pressure due to impaired aqueous humour flow from posterior chamber
- This pushes the iris forward, closing the angle between the iris and the cornea
Clinical Presentation and Diagnosis
- Risk factors: medications that dilate the pupil (anticholinergics, TCAs, antiparkinsonian drugs, etc.), family history of glaucoma, hyperopic eyes, recent eye surgery
- Diagnosis: at least 2 of following symptoms – acute onset ocular pain with nausea and vomiting, intermittent blurring of vision with halo around lights, photophobia, vision loss
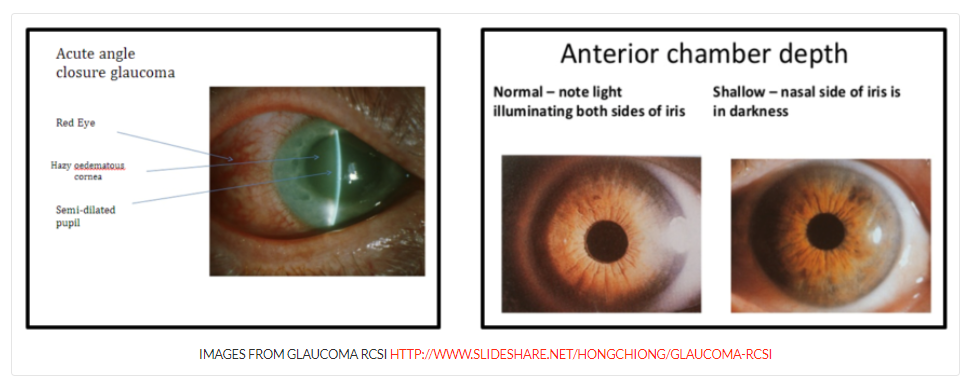
- Plus: at least 3 of following signs – intraocular pressure > 21 (typically >40), conjunctival injection, corneal epithelial edema, fixed mid-dilated pupil, shallow anterior chamber on slit lamp exam
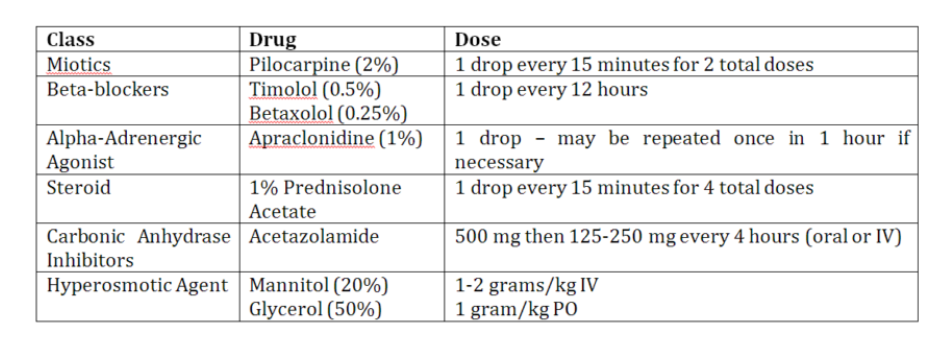
Management and medications to consider
- Consult ophthalmology (definitive management is laser iridotomy)
- Pilocarpine 1-2 drops q15min for 2 doses (miotic)
- Timolol 0.25-0.5% 1 drop (beta blocker)
- Apraclonidine drops (alpha adrenergic agonist)
- Acetazolamide 500 mg IV x 1
- Mannitol 20% 1.25-2 g/kg IV x 1
- Reassess IOP q15min in the early phases
All that follows is from Medical Concepts: Acute Angle Closure Glaucoma from CanadiEM
A 62 year old woman presents to your Emergency Department with a chief complaint of severe right eye pain. Upon further questioning, she reveals reduced vision in the affected eye and colored halos around lights. She reports a diffuse headache and two episodes of vomiting. A quick physical exam reveals significant conjunctival injection and a fixed, mid-dilated pupil. Does your differential contain acute angle closure glaucoma?
What is Acute Angle Closure Glaucoma?
Acute angle closure glaucoma is a condition characterized by raised intraocular pressure due to impaired outflow of aqueous humor from the posterior chamber of the eye.1
Clinical Presentation
As a result of the associated systemic symptoms, acute angle closure glaucoma carries a significant risk of being incorrectly diagnosed. A thorough history and physical examination with documented raised intraocular pressure is imperative for diagnosis.
History
Patients with acute angle closure glaucoma present with abrupt onset of pain in the affected eye. In addition patients may present with blurred vision, frontal headache, nausea and vomiting, photophobia, and colored halos around lights.4 Nausea and vomiting occurs as a result of autonomic stimulation, while blurred vision and colored haloes are a result of corneal edema.5 The onset is often precipitated by dilation of the pupil. When the pupil is mid-dilated, the contact between the iris and the lens is maximal and the iris thickens, which worsens pupillary block.6 Patients often describe onset of ocular pain when transitioning from a light to dark environment. Medications that dilate the pupil have the potential to precipitate an attack; these include adrenergic agents, drugs with anticholingeric effects, sulfa-based drugs, tricyclic antidepressants, anticonvulsants, and antiparkinsonian drugs.7 Other risk factors for acute angle closure glaucoma include a family history of the condition, being of Asian descent, female gender, hyperopic eyes, eyes with shallow anterior chambers, thick lens, and narrow irido-corneal angles. 6 As people age, their anterior chamber becomes more shallow and the lens thickens and moves anteriorly, 5 which makes this condition rare below the age of forty, with the peak incidence occurring in the sixth and seventh decades of life.8
Physical Examination
Patients with acute angle closure glaucoma present with conjunctival injection and a fixed, mid-dilated pupil measuring 5-6 min diameter.9 Due to the elevated intraocular pressure, the eye may feel hard to the touch. The visual acuity is often reduced. Raised intraocular pressure is necessary for the diagnosis of this condition, and is measured using a Tonopen. A pressure that exceeds 21 mmHg characterizes elevated intraocular pressure, however the pressure may exceed 60-80 mmHg. 2
Given the potentially vision compromising nature of this condition, all of these medical treatments should be initiated upon diagnosis. Intraocular pressure should be reassessed hourly to monitor response to treatment. While these pharmacological agents are often effective at lowering the intraocular pressure, patients will often require more definitive management with laser treatment, or occasionally, surgical treatment.