Another great podcast from PedsCases*: Acyanotic Congenital Heart Lesions – Part 1 Developed by Herman Bami and Dr. Michael Grattan for PedsCases.com, May 4, 2018. [Link to the podcast] [Link to the transcript].
*Here is the complete list of the Table Of Contents of the PedsCases website. On this page the site has organized all of the contents into two groups: Clinical Presentation and Specialty Area.
Here are excerpts from the podcast:
Summary
That’s the end of our first part of the podcast series on acyanotic congenital heart lesions.
The second part of this series will be focusing on outflow tract obstructions.
Before we continue on though, let’s summarize the key points from this podcast:
• Congenital heart disease is a term encompassing many pathologies and can be broadly classified into three main groups: left-to-right shunts, right-to-left shunts and outflow tract obstructions.
• Acyanotic congenital heart disease includes left-to-right shunts and outflow tract obstructions.
• Left-to-right shunts include: atrial septal defects, ventricular septal defects, patent ductus arteriosus and atrioventricular septal defects.
• The clinical presentation of these defects varies greatly based on the level of shunting and other factors, requiring careful consideration and follow-up to address present symptoms and prevent any future cardiovascular deterioration.Classification
Congenital heart disease, excluding bicuspid aortic valve, occurs in approximately 8 per 1000 births and has a broad range of clinical manifestations1. Generally, congenital heart disease is divided into cyanotic or acyanotic heart disease, a classification which is based on the level of hemoglobin saturation in the systemic circulation. Additionally, congenital heart defects can be further divided into three main pathophysiologic groups: left-to-right shunts, right-to-left shunts and outflow tract obstructions2.
Acyanotic congenital heart lesions include both left-to-right shunts and outflow tract obstructions.
Left-to-right shunts cause an increase in pulmonary circulation and include: ventricular septal defects (VSDs), atrial septal defects (ASDs), patent ductus arteriosus (PDAs), and atrioventricular septal defects (AVSDs).
On the other hand, outflow tract obstructions will usually result in normal pulmonary blood flow and include: aortic stenosis (AS), pulmonary stenosis (PS), and coarctation of the aorta.
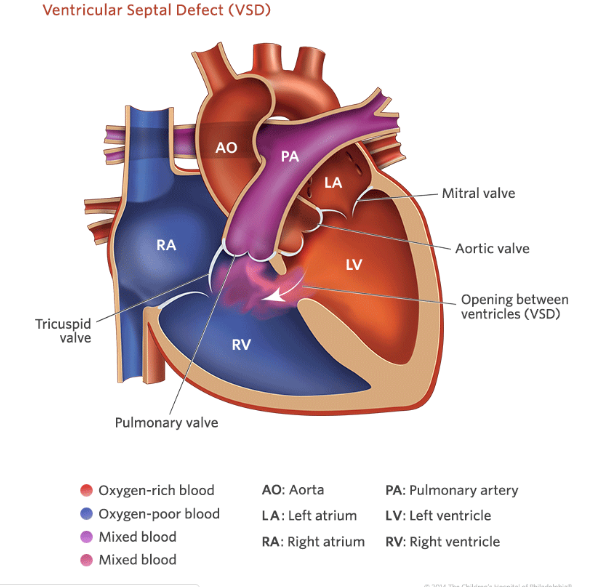
Ventricular Septal Defect
Ventricular septal defects (VSDs) are the most common congenital heart defect and comprise up to 20% of all cardiac anomalies2-3. While a VSD is a common isolated malformation, it can also be a component in several other cardiac defects that extend beyond the scope of this podcast.
. . . , the amount of flow through the VSD depends on the size of the defect and pulmonary vascular resistance (PVR). The size of the VSD also greatly effects the clinical presentation. For instance, small VSDs with little shunt can create very turbulent flow and present with a loud murmur but often be asymptomatic. Moderate to large VSDs can actually have a quieter murmur, as blood can more easily flow through a larger defect without as much turbulence. Larger defects can cause pulmonary hypertension and congestive heart failure,
and may present with fatigue, diaphoresis and respiratory distress with feedings, and failure to thrive. The typical clinical finding with a VSD would be a pansystolic murmur, usually loudest at the lower left sternal border. This murmur is secondary to left-to-right flow from the high-pressure left ventricle into the low-pressure right ventricle. Larger VSDs
are associated with higher right ventricular pressures, and do not cause pansystolic murmurs. Instead, these larger defects cause systolic ejection murmurs related to increased blood flow across the pulmonary valve. Increased flow across the mitral valve due to a large shunt may also cause a mid-diastolic rumble at the apex. Flow through the left-to-right shunt in a VSD occurs during systole when both ventricles are contracted. The contracted right ventricle acts as a conduit for blood, and an increased volume is seen in the lungs and left heart. Over time, this leads to dilation of the left heart and left ventricular
hypertrophy. A long-standing untreated VSD can also result in pulmonary hypertension leading to right ventricular hypertrophy. Significant shunts can also result in signs of
congestive heart failure including a hyperdynamic precordium, hepatomegaly and increased work of breathing.Electrocardiogram (ECG) and chest X-ray findings depend on the size of the defect.
Echocardiography can be used to provide information such as the size and location of the defect, as well as any valvular deficiencies or associated pathologies.
In terms of treatment, small VSDs usually close spontaneously and even in the absence of spontaneous closure, surgical closure of small VSDs may not be necessary. Moderate to large VSDs on the other hand may require treatment with diuretics, afterload reduction, and supplemental calories. However, the continued presence of symptoms, such as continued poor growth and pulmonary hypertension, necessitate closure. This is usually performed surgically, though some VSDs can be closed using devices placed with cardiac catheterization.
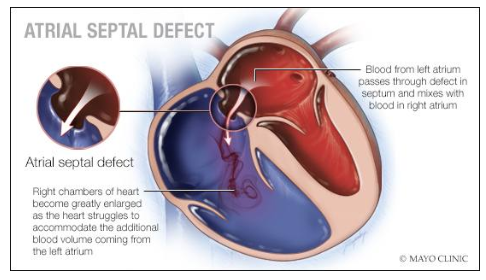
Atrial Septal Defect
Atrial septal defects (ASDs) are another type of left-to-right shunt and represent approximately 15-20% of all congenital heart defects1-2,4.
The pathophysiology and amount of shunting depend significantly on the size of the ASD and the compliance of the ventricles. The left-to-right shunt of an ASD shunts blood into a
relaxed right heart in ventricular diastole. This leads to eventual dilatation of the right heart. Even large ASDs with significant shunts are rarely symptomatic in childhood, although significant symptoms can develop in older adults including intractable arrhythmias, heart failure and more rarely, pulmonary hypertension.ECG and chest X-ray findings are a result of the increased volume in the right side of the heart and pulmonary circulation.
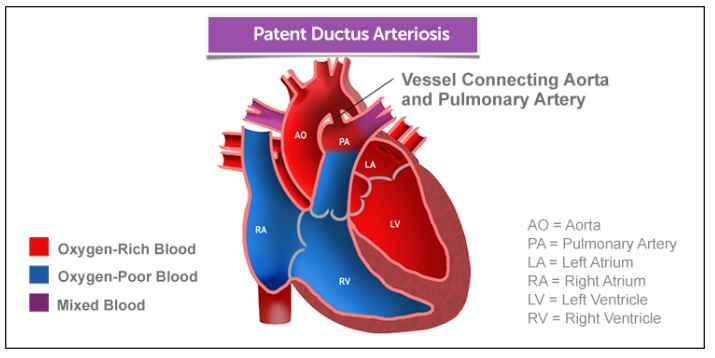
Patent Ductus Arteriosus
Patent ductus arteriosus (PDA) is a third type of left-to-right shunt and represents approximately 10 to 15% of congenital heart disease1-2,5.
It has a significantly higher prevalence in premature neonates.
Normally this [normal fetal] structure [the ductus arteriosus] spontaneously closes within 24-74 hours [of birth], however failure of this vessel to close results in a patent ductus arteriosus.
The size of the PDA as well as the pulmonary vascular resistance determine the amount of shunting that occurs, which in turn is reflected in the symptom profile.
Small PDAs are often asymptomatic but larger shunts can cause congestive heart failure* symptoms as the pulmonary vascular resistance falls. These symptoms include failure to thrive, increased work of breathing, recurrent upper respiratory tract infections and fatigue with exertion. [Poor feeding, fatigue with feeding and diaphoresis with feeding are also symptoms of congestive heart failure.]
*See Pediatric Congestive Heart Failure
Updated: Apr 23, 2019
Author: Gary M Satou, MD, FASE from emedicine.medscape.comThe murmur may only be audible in systole, or may
be absent altogether in very small PDAs or in large PDAs with associated pulmonary hypertension.Significant shunts can result in signs of congestive heart failure including a hyperdynamic precordium, hepatomegaly and increased work of breathing.
Transthoracic echocardiography is often the diagnostic method that can best determine ductal anatomy and characterize level of flow.
Spontaneous closure of a PDA is uncommon after a few weeks of age.
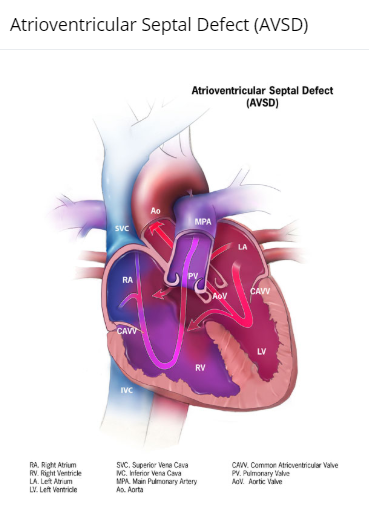
Atrioventricular Septal Defect
The fourth and last type of left-to-right shunt that we’ll be covering is atrioventricular septal defects, also known as endocardial cushion defects2,6-7. These lesions result from
failure of the septum to fuse with the endocardial cushion.The failure of the septum to properly fuse also causes abnormal atrioventricular valve development.
A complete atrioventricular septal defect involves: a primum ASD, inlet VSD, common atrioventricular valve and a tri-leaflet or cleft left atrioventricular valve. Thus, in addition to shunting, there may be atrioventricular valve insufficiency.
There is a strong association between AVSD and trisomy 21 or Down’s syndrome. AVSD is the most common congenital heart defect in infants with Down syndrome and 40-50% of infants with AVSD identified prenatally will go on to have Down syndrome.
As the pulmonary vascular resistance falls over the first few months of life, congestive heart failure symptoms* such as increased work of breathing, fatigue and failure to thrive
can develop. This is mainly due to the VSD, although atrioventricular valve insufficiency can exacerbate these symptoms. The presence of other signs, such as murmurs, depends on the level and extent of the shunting in both the atrial and ventricular defects.*See Pediatric Congestive Heart Failure
Updated: Apr 23, 2019
Author: Gary M Satou, MD, FASE from emedicine.medscape.comDiagnosis of atrioventricular defects is normally made with echocardiography, which can also be used to better identify the appropriate therapeutic intervention.
Additional Resources:
(1) Pediatric Congestive Heart Failure. Updated: Apr 23, 2019.
Author: Gary M Satou, MD, FASE from emedicine.medscape.com