This post contains links to and excerpts from Resource (1) below, Angioedema in the emergency department: a practical guide to differential diagnosis and management.
Here are some excerpts:
Abstract
Background: Angioedema is a common presentation in the emergency department (ED). Airway angioedema can be fatal; therefore, prompt diagnosis and correct treatment are vital.
Objective of the review: Based on the findings of two expert panels attended by international experts in angioedema and emergency medicine, this review aims to provide practical guidance on the diagnosis, differentiation, and management of histamine- and bradykinin-mediated angioedema in the ED.
Review: The most common pathophysiology underlying angioedema is mediated by histamine; however, ED staff must be alert for the less common bradykinin-mediated forms of angioedema. Crucially, bradykinin-mediated angioedema does not respond to the same treatment as histamine-mediated angioedema. Bradykinin-mediated
angioedema can result from many causes, including hereditary defects in C1 esterase inhibitor (C1-INH), side effects of angiotensin-converting enzyme inhibitors (ACEis), or acquired deficiency in C1-INH. The increased use of ACEis in recent decades has resulted in more frequent encounters with ACEi-induced angioedema in the ED; however, surveys have shown that many ED staff may not know how to recognize or manage bradykinin-mediated
angioedema, and hospitals may not have specific medications or protocols in place.
Conclusion: ED physicians must be aware of the different pathophysiologic pathways that lead to angioedema in order to efficiently and effectively manage these potentially fatal conditions.
Keywords: Angioedema, Emergency department, Histamine-mediated, Bradykinin-mediated, Guideline
Background
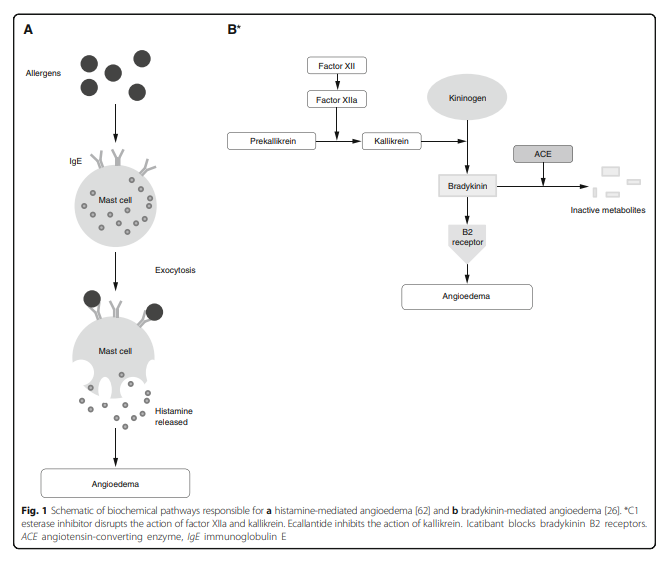
Angioedema is mediated by several mechanisms, including histamine and bradykinin (Fig. 1[above]). Diagnosis of the specific type of angioedema is essential for appropriate treatment [3]; however, many ED physicians may not know how to distinguish different types of angioedema or how to effectively treat less common presentations [4].
Hospitalization can be used as a proxy measure of the severity of angioedema. Patients with undifferentiated angioedema (i.e., including both histamine- and bradykininmediated angioedema) visiting the ED are admitted for inpatient care (11% of ED visits) more frequently than patients with allergic reactions (2.2% of ED visits) [2, 5]. Hospitalization rates following ED visits for HAE (45–50%) and ACEi-induced angioedema (42–66%) are even higher [5, 6, 10, 12]. Hospitalizations for angioedema have increased over the last 15 years, from 3.3 to 3.4:100,000 admissions in 1998–2000 to 4.0:100,000 in 2005 and 5.4:100,000 in 2009 [15, 16]. The rise is thought to be related to increased prescribing of ACEis over this time period [15, 16].
Mortality data for angioedema are lacking; however, one study demonstrated a small but ever-present risk of death by asphyxiation in patients with HAE with development of fatal laryngeal attacks within as little as 15 min [17]. Crucially, the risk of death is three- to nine-fold higher in patients who have not received a confirmed diagnosis of
HAE, emphasizing the importance of preparation and awareness in preventing adverse outcomes [17]. Although angioedema with a well-defined bradykinin-mediated pathogenesis is relatively rare, most ED staff will likely encounter a case at some point in their career. Therefore, awareness of bradykinin-mediated angioedema is important.Because bradykinin-mediated angioedema is uncommon, there generally are not protocols in place in the ED and there is a lack of immediate access to appropriate drugs for bradykinin-mediated angioedema. For example, a recent survey of British EDs demonstrated that medications required to treat bradykinin-mediated angioedema were available in the majority of hospitals with specialist immunology services, but were not readily accessible in the ED (e.g., located in the main pharmacy). Additionally, only half the hospitals surveyed had established guidelines for the use of these medications [18].
Lack of protocols and access to medications can lead
to treatment errors and poor outcomes for ED patients presenting with bradykinin-mediated angioedema [19, 20]. This paper reports the findings and recommendations of two expert panels of 16 international experts in angioedema and emergency medicine convened during 2013 [21, 22]. The aim of this paper is to provide practical guidance on the early identification of bradykinin-mediated angioedema in the ED to improve the diagnosis and outcomes of angioedema attacks.Review
Start here on p 3 of the PDF.
(1) Angioedema in the emergency department: a practical guide to differential diagnosis and management [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Int J Emerg Med. 2017 Dec;10(1):15.