The big problem in weight loss diet therapies is thought to be the decline in the resting metabolic rate (RMR) with calorie restriction and weight loss. This is thought to be the reason for the failure of many persons to successfully keep off the weight they have lost with diet therapy.
Resource (1) below is a helpful introduction to the problems associated with maintaining weight loss achieved by caloric restriction diets. The article has been cited by 11 articles indexed in PubMed and in one systematic review. The following are excerpts from this article:
Despite years of research, the treatment of obesity continues to revolve around the seemingly simple concept of balancing calorie expenditure with calorie intake. However, the determinants of energy expenditure, specifically resting metabolic rate, are an active area of research with many debatable issues. This review will address the calorie expenditure side of the scale, with the examination of the effect of dieting and exercise on resting metabolic rate. Resting metabolic rate accounts for 60–75% of total energy expenditure in sedentary people.2 Therefore, it is a major determinant of energy balance and changes in weight. Factors which decrease resting metabolic rate would be associated with difficulty maintaining weight or weight loss, or frank weight gain. On the contrary, anything that increases resting metabolic rate would facilitate weight loss and maintenance of weight loss. Caloric restriction is known to produce a short-term reduction in resting metabolic rate. Issues that have not been resolved regarding such a reduction are as follows: is the reduction proportional to the reduction in body size or the degree of energy deficit, is the reduction permanent or self-limiting, and can exercise prevent the reduction? If this reduction is a permanent reduction in resting metabolic rate, and if it is above and beyond what would be predicted by the resulting smaller body size, then weight loss after calorie restriction will be very difficult to maintain. This paper reviews four articles that address these issues, three reports of primary research and one meta-analysis. Concluding remarks follow regarding actions that primary care physicians can take in the assessment and treatment of obesity.
Family practice physicians can facilitate healthy and successful weight management among their patient populations by heeding the following tips: (i) determine long-term weight goals based on obtaining a body mass index under 27, if possible 25; (ii) determine short-term weight goals based on a reduction of 1 to 2 body mass index units (approximately 4.5–7.3 kilograms or 10–16 pounds); (iii) encourage patients to maintain this interim goal for 6 months to allow for readjustment of resting metabolic rate for new body mass (as well as for psychosocial adjustments and commitment to necessary behaviour changes); and (iv) determine the next short-term weight goal. Continue to support patient through this cyclical process until body mass index is at least under 27, if not at 25.7 The physician will also need to explore appropriate nutrition and exercise education and counselling options with the patients, based on the patient’s resources, education level and learning style. Based on patients’ medical history and preferences, appropriate individualized diet and exercise prescriptions should be developed. This is best approached with a health care team including a physician, registered dietitian and exercise physiologist. Through this slow and thought-ful process of cycles of weight loss and weight maintenance it is thought that patients will be able to prevent the more debilitating cycles of rapid weight loss, short-term reductions in metabolic rate and rapid weight gain.
The following article, Resource (2) below, addresses a possible way to prevent decline in the RMR and hopefully prevent the regain of lost weight.
Abstract
Background: The resting metabolic rate (RMR) decrease, observed after an obesity reduction therapy is a determinant
of a short-time weight regain. Thus, the objective of this study was to evaluate changes in RMR, and the associated
hormonal alterations in obese patients with a very low-calorie ketogenic (VLCK)-diet induced severe body weight
(BW) loss.Method: From 20 obese patients who lost 20.2 kg of BW after a 4-months VLCK-diet, blood samples and body
composition analysis, determined by DXA and MF-Bioimpedance, and RMR by indirect calorimetry, were obtained
on four subsequent visits: visit C-1, basal, initial fat mass (FM) and free fat mass (FFM); visit C-2, − 7.2 kg in FM, − 4.
3 kg in FFM, maximal ketosis; visit C-3, − 14.4 kg FM, − 4.5 kg FFM, low ketosis; visit C-4, − 16.5 kg FM, − 3.8 kg FFM, no
ketosis. Each subject acted as his own control.Results: Despite the large BW reduction, measured RMR varied from basal visit C-1 to visit C-2, − 1.0%; visit C-3, − 2.4%
and visit C-4, − 8.0%, without statistical significance. No metabolic adaptation was observed. The absent reduction in
RMR was not due to increased sympathetic tone, as thyroid hormones, catecholamines, and leptin were reduced at
any visit from baseline. Under regression analysis FFM, adjusted by levels of ketonic bodies, was the only predictor of
the RMR changes (R2 = 0.36; p < 0.001).Conclusion: The rapid and sustained weight and FM loss induced by VLCK-diet in obese subjects did not induce the
expected reduction in RMR, probably due to the preservation of lean mass.Trial registration: This is a follow up study on a published clinical trial.
Keywords: Ketogenic diet, Very low-energy diet, Pronokal method, Protein diet, Obesity, Metabolic adaptation, Energy
expenditure, Indirect calorimetry, DXA, Multifrequency BIABackground
It is widely accepted that during periods of energy deficit
or restriction (eg., weight-loss diets), the human body
tends to diminish energy expenditure by increasing the efficiency in its use and by decreasing the resting metabolic
rate (RMR) [18]. This phenomenon of metabolic adaptation
to weight reduction is called adaptive thermogenesis, defined as a decrease in RMR out of proportion to the decrease
in body mass [5, 12]. Various groups have observed
this phenomenon during obesity treatments independently
of the strategy employed, including diet, exercise,
diet plus exercise, pharmacologic treatments, and surgical
interventions, and suggest that metabolic adaptation predisposes weight reduced obese patients to weight regain.Published research has shown that a very low calorie
ketogenic (VLCK)-diet was able to induce a significant
weight loss and maintained their efficacy along 2 years
[10, 11]. Because VLCK-diets target body fat mass (FM)
with little reduction in fat free mass (FFM) [6], the
working hypothesis was that VLCK-diet may induce a
minor or null reduction in the RMR, thus preventing
body weight regain.Nutritional intervention
All the patients followed a VLCK diet according to a
commercial weight loss program (PNK method®) [Resource (4) below], which includes lifestyle and behavioral modification support. The intervention included an evaluation by the specialist physician conducting the study, an assessment by an expert dietician, and exercise recommendations. This method is
based on a high-biological-value protein preparations obtained
from cow milk, soya, avian eggs, green peas and cereals. Each protein preparation contained 15 g protein, 4 g carbohydrates, 3 g fat, and 50 mg docohexaenoic acid, and provided 90–100 kcal.The weight loss program has five steps (Additional file 1:
Figure S1) [Resource (2a) below] and adheres to the most recent guidelines of 2015 European Food Safety Authority (EFSA) on total carbohydrates intake [3] [Resource (3a)]. The first three steps consist of a VLCK diet (600–800 kcal/day), low in carbohydrates (< 50 g daily from vegetables) and lipids (only 10 g of olive oil per day). The amount of high-biological-value proteins ranged between 0.8 and 1.2 g per each kg of ideal body weight, to ensure patients were meeting their minimal body requirements and to prevent the loss of lean mass.In step 1, the patients ate high-biological-value protein
preparations five times a day, and vegetables with low glycemic
indexes.In step 2, one of the protein servings was
substituted by a natural protein (e.g., meat or fish) either
at lunch or at dinner.In step 3, a second serving of low fat natural protein was substituted for the second serving of biological protein preparation. Throughout these ketogenic phases, supplements of vitamins and minerals supplements, such as K, Na, Mg, Ca, and omega-3 fatty acids, were provided in accordance to international recommendations [22]. These three steps were maintained until the patient lost the target amount of weight, ideally 80%. Hence, the ketogenic steps were variable in time depending on the individual and the weight loss target.
In steps 4 and 5, the ketogenic phases were ended by
the physician in charge of the patient based on the amount
of weight lost, and the patient started a low-calorie diet
(800–1500 kcal/day). At this point, the patients underwent
a progressive incorporation of different food groups and
participated in a program of alimentary re-education to
guarantee the long-term maintenance of the weight loss.
The maintenance diet, consisted of an eating plan balanced
in carbohydrates, protein, and fat. Depending on the individual
the calories consumed ranged between 1500 and
2000 kcal/day, and the target was to maintain the weight
lost and promote healthy life styles.During this study, the patients followed the different
steps of the method until they reach the target weight or
up to a maximum of 4 months of follow-up, although
patients remained under medical supervision for the following
months.Anthropometric assessment
All anthropometric measurements were undertaken after
an overnight fast (8 to 10 h), under resting conditions,
in duplicate, and performed by well-trained health
workers. . . . BMI was calculated by dividing
body weight in kilograms by the square of height in
meters (BMI = weight (kg)/height2 (m).Resting metabolic rate
The RMR was measured by indirect calorimetry using a
portable desktop metabolic system (FitMate PRO, Cosmed,
Rome, Italy) and under overnight fasting conditions.The FitMate uses a turbine flow meter for measuring ventilation
and a galvanic fuel cell oxygen sensor for determining the
fraction of oxygen in expired gases. Moreover, it has sensors
for the measurement of temperature, humidity, and barometric
pressure for use in internal calculations. The FitMate
uses standard metabolic formulas to estimate oxygen
consumption, and RMR is calculated using a predetermined
respiratory quotient (RQ) of 0.85. During the measurement
period, participants remained sitting, breathed normally, and were instructed to remain awake, and to avoid talking, fidgeting and hyperventilating. The reliability of measuring RMR with Cosmed’s FitMate metabolic system have been determined in several previous studies [9, 15, 21], and by in house controls (Additional file 2: Figure S2) [Resource (2b) below].Total body composition
Body composition was first measured by dual-energy X-ray
absorptiometry (DXA; GE Healthcare Lunar, Madison,
USA).Daily quality control scans were acquired during the
study period. No hardware or software changes were made
during the course of the trial. Subjects were scanned using
standard imaging and positioning protocols, while wearing
only light clothing. For this study, the values of bone
mineral density, lean body mass and FM that were directly
measured by the GE Lunar Body Composition
Software option. Some derivative values, such as bone
mineral content, regional lean mass, FFM, and fat mass
percentage (FM%), were also calculated.Multifrequency bioelectrical impedance
Multifrequency bioelectrical impedance (MF–BiA) was
also used for determining body composition. FM, FM%,
FFM, total body water, intra- and extracellular water, and
skeletal muscle mass, were calculated with In Body 720
(In Body 720, Biospace Inc.,Tokyo, Japan). This technology
is non-invasive and uses eight contact electrodes, which
are positioned on the palm and thumb of each hand and
on the front part of the feet and on the heels.Determination of levels of ketone bodies
Ketosis was determined by measuring ketone bodies, specifically
β-hydroxy-butyrate (β-OHB), in capillary blood by
using a portable meter (GlucoMen LX Sensor, A. Menarini
Diagnostics, Neuss, Germany). As with anthropometric assessments, all the determinations of capillary ketonemia
were made after an overnight fast of 8 to 10 h. These measurements were performed daily by each patient during the
entire VLCK diet, and the corresponding values were
reviewed on the machine memory by the research team in
order to control adherence. Additionally, β-OHB levels
were determined at each visit by the physician in charge
of the patient. The measurements reported as “low value”
(< 0.2 mmol/l) by the meter were assumed as to be zero
for the purposes of statistical analyses.Biochemical parameters
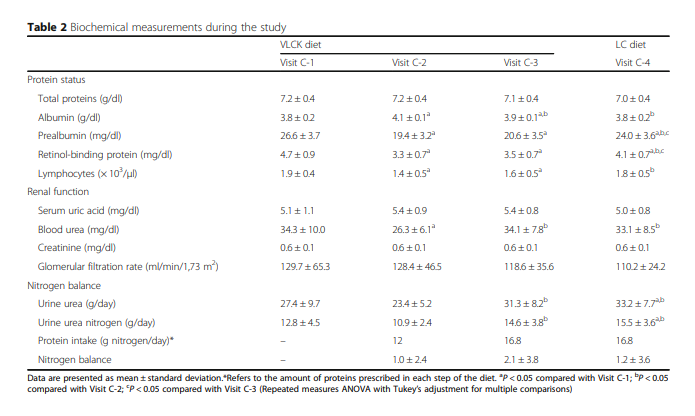
During the study all the patients were strictly monitored
with a wide range of biochemical analyses. However, for
the purposes of this work only certain values are reported. Serum tests for total proteins, albumin, prealbumin,
retinol-binding protein, red cell and white cells counts,
uric acid, urea, creatinine and urine urea were performed
using an automated chemistry analyzer (Dimension EXL
with LM Integrated Chemistry System, Siemens Medical
Solutions Inc., USA).Thyroid-stimulating hormone (TSH),
free thyroxine (FT4), and free triiodothyronine (FT3)
were measured by chemiluminescence using ADVIA
Centaur (Bayer Diagnostics, Tarrytown, NY, USA). All
the biochemical parameters were measured at the 4
complete visits.The overnight fasting plasma levels of leptin were measured
using commercially available ELISA kits (Millipore, MA, USA). The fasting plasma levels of fractionated catecholamines
(dopamine, adrenaline and noradrenaline) were tested by high pressure liquid chromatography (HPLC; Reference Laboratory, Barcelona, Spain).Results
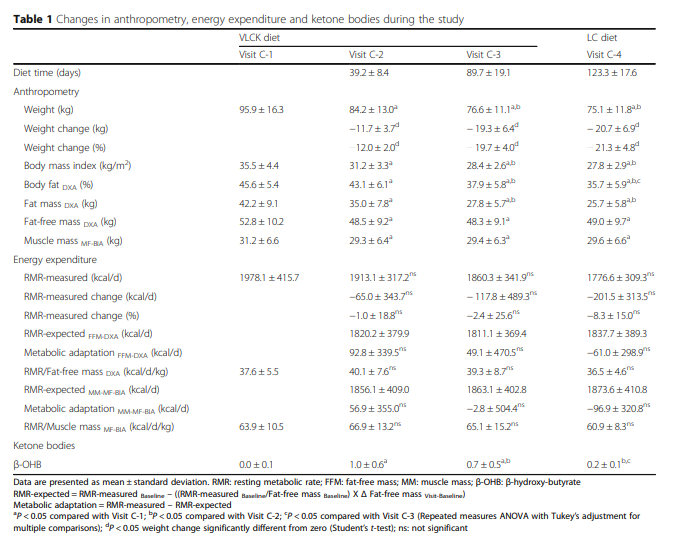
Twenty obese patients, 12 females, age from 18 to 58 years
(47.2 ± 10.2 yr) completed the study. Participants at baseline
have a BMI of 35.5 ± 4.4 and body weight (BW) of
95.9 ± 16.3 kg, 45.6 ± 5.4% of which was fat.Although the patients underwent a total of 10 visits, the
RMR and body composition analyses were synchronized
with the ketone levels in four visits (Fig. 1a). Visit C-1 was
the baseline visit, before starting the diet and with no ketosis
(0.0 ± 0.1 mmol/L) and initial weight. Visit C-2 was at
the time of maximum level of ketosis (1.0 ± 0.6 mmol/L)
with 11.7 kg of BW loss. At visit C-3 (after 89.7 ± 19.1 days
of VLCK), patients started the return to a normal diet and
showed a reduction in ketone levels (0.7 ± 0.5 mmol/L)
with 19.3 kg of BW loss. Finally, at visit C-4 the patients
were out of ketosis (0.2 ± 0.1 mmol/L) with a total of
20.8 kg of weight lost (Table 1 and Fig. 1).Most of the initial BW loss was in the form of fat mass
(FM) with a minor reduction in fat free mass (FFA). The
reduction in kg for FM and FFM respectively from baseline
were; visit C-2 7.2 kg and 4.3 kg; visit C-3 14.4 kg and
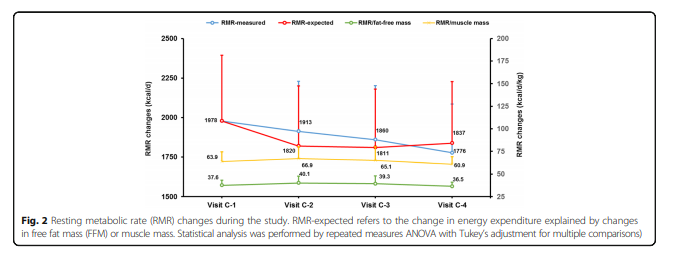
4.5 kg; visit C-4 16.5 kg and 3.8 kg. (Table 1, Fig. 1b).The measured RMR was not significantly different from
the baseline at any time during the study, although a
downward trend in these values was observed (Fig. 2a).
The following paragraph is interesting and a little concerning about whether or not the trend towards decreased RMR was significant (the authors state that the decrease in RMR was not statistically significant).
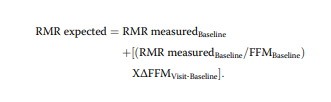
To investigate how much of the mild and non-significant
decrease in RMR could be accounted for by FFM change,
we used the baseline RMR data to generate an equation for
calculating the expected-RMR in accordance with variations
in FFM (Table 1). The difference between the measured
and expected RMR defined the degree of metabolic
adaptation. At visit C-2 (maximum ketosis), the measured
RMR was 92.8 ± 339.5 kcal/d higher than expected RMR.
At visit C-3, the measured RMR was 49.1 ± 470.5 kcal/d
greater than expected RMR. Finally, at visit C-4, the measured RMR was 61.0 ± 298.9 kcal/d lower than the expected
RMR. None of the differences between the measured
and expected RMR was statistically different (Fig. 2
and Table 1), indicating that the phenomenon of metabolic
adaptation was not present.The observation that the VLCK-diet preserved the RMR in accordance to variations in FFM, thus avoiding the
metabolic adaptation was reinforced by the maintenance
of the RMR/FFM quotient during the study (Table 1
and Fig. 2). When, muscle mass evaluated by MF-BiA
was employed in the analysis, instead of DXA, results
on the expected and observed RMR were similar
(Table 1 and Fig. 2).Discussion
To the best of our knowledge this study is the first assessing
the effect of VLCK-diet on the RMR of obese patients.
The main findings of this work were: 1) the rapid
and sustained weight reduction induced by the VLCK diet
did not induce the expected drop in RMR, 2) this observation was not due to a sympathetic tone counteraction through the increase of either catecholamines, leptin or thyroid hormones, 3) the most plausible cause of the null reduction of RMR is the preservation of lean mass (muscle mass) observed with this type of diet.The greatest challenge in obesity treatment is to avoid
weight recovery sometime after the previous reduction.
In fact, after one or few years the most obese patients recover
or even increase their weight, previously reduced by
either, dietetic, pharmacological or behavioral treatments
[8], bariatric surgery being the only likely exception [7].
Since obesity reduction is accompanied by a slowing of
energy expenditure in sedentary individuals, mostly RMR,
this fact has been blamed for this negative outcome of the
diet-based treatments [12]. RMR is recognized as the major component of total energy expenditure, being responsible
for about 75% of daily total energy expenditure in Western
societies [1, 16]. Therefore any RMR reduction after treatment,
translates in a large impact on energy balance, making
subjects more prone to weight regain over time [17].
This phenomenon was called metabolic adaptation or adaptive
thermogenesis, indicating that RMR is reduced after
weight loss, and furthermore that this reduction is usually
larger than expected or out of proportion with the decrease
in fat or fat free mass [2].Therefore, preservation of initial
RMR after weight loss could play a critical role in facilitating
further weight loss and preventing weight regain in the
long-term [4].We have observed that the obesity-reduction by a VLCKdiet
(Pnk method ®) was maintained 1 and 2 years after its
completion [10, 11].
Resources:
(1) Selections From The Current Literature: Effects of dieting and exercise on resting metabolic rate and implications for weight management [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Fam Pract. 1999 Apr;16(2):196-201.
This article has been cited by one 2013 systematic review article and has been cited by eleven articles indexed in Pubmed.
(2) Resting metabolic rate of obese patients under very low calorie ketogenic diet [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Nutr Metab (Lond). 2018; 15: 18.
Published online 2018 Feb 17. doi: 10.1186/s12986-018-0249-z
Additional Files For The Above Article
(2a) Additional file 1: Figure S1. Nutritional intervention program and
schedule of visits. Visit C-4 was performed at the end of the study according
to each case, once the patient achieved the target weight or maximum at
4 months of follow-up. (PDF 390 kb)
(2b) Additional file 2: Figure S2. Bland Altman plots of Resting Metabolic Rate
(RMR) for Cosmed’s Fitmate device compared to the Deltatrac. (PDF 11 kb)
(2c) Additional file 3: Table S1. Independent effects of fat-free mass, free
triiodothyronine, catecholamines, leptin and β-hydroxy-butyrate on resting
metabolic rate at each visit. (DOCX 32 kb)
(3) PnK® Method Website:
Lipoinflammation is an inflammatory process of the cells in fatty tissue, leading to a chronic inflammatory state in obese or overweight people. The inflammation is not visible from the outside, but it is directly linked to obesity and a tendency to regain weight after a diet.
The New PnK® Method is a medical weight-loss treatment designed specifically to solve lipoinflammation, helping to:
- Lose weight safely and efficiently in the short term.
- See the whole treatment through, from beginning to end.
- Not regain the weight lost.
(4) Body Composition Changes After Very-Low-Calorie Ketogenic Diet in Obesity Evaluated by 3 Standardized Methods [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Endocrinol Metab. 2017 Feb 1;102(2):488-498. doi: 10.1210/jc.2016-2385.
(4) Scientific Opinion on the essential composition of total diet replacements
for weight control [Full Text PDF]. EFSA Journal 2015;13(1):3957.
(5) Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Gastroenterology. 2017 May;152(7):1718-1727.e3. doi: 10.1053/j.gastro.2017.01.052. Epub 2017 Feb 11.
(7) Metabolic slowing with massive weight loss despite preservation of fat-free mass [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Endocrinol Metab. 2012
(8) Weight Loss and Health Status 3 Years after Bariatric Surgery in Adolescents [PubMed Abstract] [Full Text HTML] [Full Text PDF]. N Engl J Med. 2016 Jan 14;374(2):113-23. doi: 10.1056/NEJMoa1506699. Epub 2015 Nov 6.