Emergency Medicine Cases Episode 60: Emergency Management of Hyponatremia is outstanding and every clinician needs to review the podcast and show notes.
Here is the link to the PDF show notes. And here are some excerpts from the start of the PDF:
Hyponatremia is the most common fluid and electrolyte disorder encountered in clinical practice and is found in approximately 20% of admissions to hospital. In addition to being extremely prevalent, hyponatremia is an independent predictor of MORTALITY. There is a clear, linear relationship between serum sodium <135 mmol/L at the time of admission to hospital and IN HOSPITAL mortality. Efforts to reverse hyponatremia can also be dangerous for the patient. Under correction of serum sodium can lead to the development of cerebral edema whereas rapid over-correction of serum sodium can put patients at risk for Osmotic Demyelination Syndrome (ODS)- formerly known as Central Pontine Myelinolysis. There are two factors which influence how symptomatic a patient will be from their hyponatremia: severity of hyponatremia and the acuity of onset. The lower the sodium and the faster the fall, the more symptomatic a patient will become. Symptoms are often vague and non-specific presenting as headache, irritability, lethargy, confusion, agitation or unstable gait leading to a fall.
From the podcast and show notes:
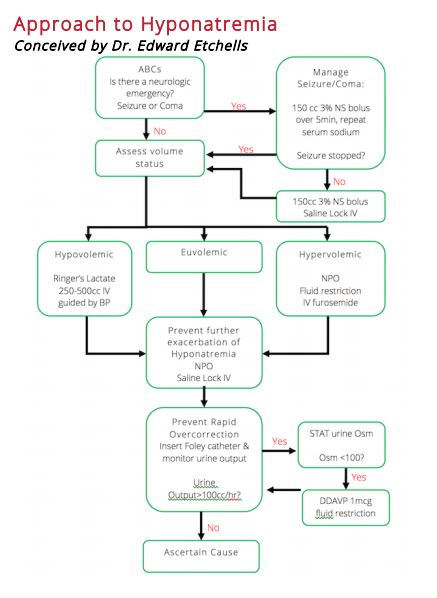
In this EM Cases episode Dr. Melanie Baimel and Dr. Ed Etchells discuss a simple and practical step-wise approach to the emergency management of hyponatremia:
1. Treat neurologic emergencies related to hyponatremia with hypertonic saline
2. Defend the intravascular volume
3. Prevent worsening hyponatremia
4. Prevent rapid overcorrection with the Rule of 100s
5. Ascertain the cause
Dr. Etchells and Dr. Baimel answer questions such as: What are the indications for giving DDAVP in the emergency management of hyponatremia? What is a simple and practical approach to determining the cause of hyponatremia in the ED? How fast should we aim to correct hyponatremia? What is the best fluid for resuscitating the patient in shock who has a low serum sodium? Why is the management of exercise associated hyponatremia counter-intuitive? What strategies can we employ to minimize the risk of Osmotic Demyelination Syndrome (OSD) and cerebral edema in the emergency management of hyponatremia? and many more…