In this post I link to and excerpt from Emergency Medicine Cases’ ECG Cases 19 Tachycardias – Approach, WIDER Mnemonic for Wide SVT DDx, VT vs SVT, March 2021.
Note to myself when reviewing: First review the notes below from Dr. McClaren’s post and then go to the post to test myself by reviewing the ten ECGs he has provided for us.
All that follows is from the above:
An Approach to Tachycardias
The management of tachycardia (HR>100 in adults) depends on the ECG and the patient:
- Sinus tachycardia (P waves before every QRS, upright in in I and II): treat underlying cause
- Unstable
- from non-sinus tachycardia: electrical cardioversion
- unrelated to non-sinus tachycardia: treat underlying +/- rate/rhythm
- Stable non-sinus tachycardia
- Narrow QRS (<120ms)
- Irregular
- Different P wave morphologies = MAT: treat underlying, magnesium
- Flutter waves = atrial flutter with variable block: treat underlying, rate/rhythm control
- No P/flutter waves = atrial fibrillation: treat underlying, rate/rhythm control
- Regular
- Flutter waves = atrial flutter with fixed block: treat underlying, rate/rhythm control
- No preceding P/flutter waves = SVT: vagal, adenosine, CCB, cardiovert
- Wide QRS (>120ms)
- Irregular
- Afib/flutter with BBB: treat underlying, rate/rhythm control
- AF + WPW: procainamide, electrical cardioversion
- Polymorphic VT: electrical cardioversion, amiodarone if normal QT, magnesium if long QT
- Regular: monomorphic VT vs SVT: adenosine, procainamide, electrical cardioversion
The first step is to identify sinus tachycardia because the management—whether the patient is stable or unstable, and whether the QRS is narrow or wide—is to identify and treat the underlying cause. Because P waves are small and can be confused with T waves, U waves, flutter waves or artifact, computer interpretation often fails at rhythm analysis [1]. But remembering anatomy can help: sinus conduction begins in the upper right atrium and spreads down and to the left, so look at V1 for biphasic P waves and lead II for upright P waves.
If the tachycardia is not sinus, then the next step is to assess clinical stability and consider electrical cardioversion. If a patient is clinically unstable as a result of non-sinus tachycardia, then the management—whether narrow complex like SVT or AF, or wide complex like VT or SVT with abberancy—is immediate electrical cardioversion. On the other hand, a patient’s instability might be unrelated to their tachycardia (eg chronic atrial fibrillation with hypotension from sepsis), requiring treatment of the underlying cause with or without managing their arrhythmia.
If the patient has a non-sinus tachycardia but is stable, then further analysis of the ECG can identify the specific arrhythmia and guide management—based on QRS width, regularity and atrial activity. Narrow complex tachycardia (QRS<120ms) indicates normal ventricular conduction and therefore a supraventricular source of arrhythmia. As with sinus rhythm, leads V1 and II are helpful to identify flutter waves, which most commonly proceed in a counter-clockwise loop away from lead II (producing inverted flutter waves) and towards V1 (producing upright flutter waves mimicking P waves). Wide complex tachycardia (QRS>120) can be either supraventricular (with abnormal conduction, from a variety of possible reasons) or ventricular in origin. As a review article summarized, “A large body of discussion has focused on the 2 major types of WCT: ventricular tachycardia (VT) and paroxysmal supraventricular tachycardia (PSVT) with aberrancy. However, there are several other important causes of a WCT encountered in clinical practice, which are less often discussed. These tachycardias are abnormal, often requiring specific therapies differing from the standard approach to WCT.”[2] The differential for supraventricular rhythms that have wider QRS complexes can be remembered by the mnemonic WIDER.
WIDER Mnemonic for DDx SVT with Wide QRS
- WPW + AF: very rapid, irregular and variable complexes: procainamide or electrical cardioversion
- Intraventricular conduction delay: pre-existing or rate-related BBB: treat underlying
- Drugs: sodium channel blocker (sinus tach, QRS>100 and possibly very wide, right axis, tall R in aVR): sodium bicarb
- Electrolytes: hyperkalemia (long PR or junctional rhythm, prolonged QRS, peak T, “slow VT” or “very wide VT”): calcium, glucose/insulin
- Raised ST segments (STEMI) producing pseudo-QRS widening: reperfusion
If the differential is narrowed down to VT vs SVT with aberrancy, there’s an 80% pre-test likelihood of VT, even higher in older patients with CAD. There are certain criteria that can further suggest VT—based on VT originating in the ventricles independently of the atria, and propagating through delayed conduction in an abnormal direction:
- Heart rate/rhythm: AV dissociation, caption/fusion beats
- Electrical conduction:
- prolonged conduction: QRS>140, RS>100, R-wave peak>50ms in lead II
- morphology
- Atypical LBBB: V1 r>30ms, RS>60, notched S; V6 Q wave
- Atypical RBBB: V1 monophasic R or R>R’; V6 R:S<1
- Axis: extreme axis deviation, axis change from baseline
- R-wave: precordial concordance (all precordial leads have either positive concordance or negative concordance); absence of RS complex in precordial leads; monophasic R in aVR
But as a review summarized, “While all have proven their value in distinguishing VT and SWCT, no single criterion or collection of criteria promises diagnostic certainty.”[3] Fascicular VT, for example, originates and uses the ventricular conducting system, so can give a typical aberrant morphology and can be found in young patients without heart disease (idiopathic VT). In the unstable patient it’s a moot point because they require immediate electrical cardioversion. In the stable patient with regular monomorphic WCT, adenosine is included in the guidelines as a therapeutic test (but not a diagnostic test, as some VT respond to adenosine). But “when doubt exists, it is safest to assume that any wide-complex tachycardia is VT, particularly in patients with known cardiovascular disease” and treat accordingly: procainamide or electrical cardioversion.[4]
ST changes can be secondary to the tachycardia itself, secondary to abnormal conduction, a primary abnormality from ischemic, metabolic or toxic causes—or a combination. So analysis of the ST segment and T waves needs to be put in context of the rest of the ECG, and the patient.
Now go to Dr. McClaren’s post and test yourself against his ten ECGs.
And when you analyze the ECG, use the H E A R T S template to analyze the rhythm.
So, the first time through, I’m going to go thru the H E A R T S template answer for each of the ten ECGs. So go to the post and to the second ten ECGs after Dr. McClaren’s great tachycardia review notes. I’ll list the ten H E A R T S template answers for my review.
Case 1: 25yo found confused with an empty bottle of pills. HR 130 BP 150/90 R20 sat 97% temp 38.0
Case 1: sinus tachycardia from TCA-type OD
- Heart rate/rhythm: sinus tach (biphasic seen clearly in V1, and upright P superimposed on T wave in lead II)
- Electrical conduction: borderline QRS (100ms), long QT (580ms)
- Axis: incomplete RBBB*, borderline right axis
- R-wave: delayed R wave progression, tall terminal R in aVR
- Tension: no hypertrophy
- ST/T: no changes
Impression: TCA-type OD (from benadryl OD): sinus tach, sodium channel blockade (borderline QRS, S wave in I, tall R wave in aVR) and prolonged QT. Treated with fluids, sodium bicarb and magnesium, with resolution of changes.
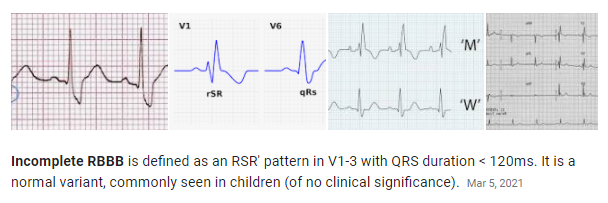
*Incomplete Right Bundle Branch Block from Right Bundle Branch Block (RBBB)
Ed Burns and Robert Buttner Mar 5, 2021 from Life In The Fast Lane:
*See also Electrical Right and Left Axis Deviation, by StatPearls, January 24, 2021. This resource has lists of the causes of right and left axis deviation.
Case 2: 75yo with sudden palpitations. HR 210 BP 110/70 R18 sat 98%
Case 2: SVT with rate-related ST changes