After reviewing this resource, be sure and review The Curbsiders’ #361 Advanced Lipidology With Erin Michos, MD
Posted on October 26, 2022, by Tom Wade MD
Prior lipid episodes:
#37 Lipids, PCSK9, and ezetimibe: Lower is better.
#10 Cholesterol, lipids, statins, fish oil. Become a Master Lipidologist.
In this post I link to and excerpt from the Curbsiders‘ [Link is to the episode list] podcast and show notes from #191 Lipids Update and Cardiovascular Risk Reduction with Erin Michos MD: PRIMARY AND SECONDARY PREVENTION OF CARDIOVASCULAR DISEASE. JANUARY 20, 2020 By DR. CHRIS CHIU.
All that follows is from the above podcast and show notes.
Lipids Update! Get up close and personal with ASCVD prevention and lipid management guidelines, including changes in the 2018 update, with our discussion with Dr. Erin Michos @erinmichos, preventive cardiologist and associate professor of medicine at the Johns Hopkins University Hospital!
Time Stamps
- 00:00:00 Intro
- 00:01:52 Getting to know Dr. Erin Michos
- 00:O6:50 Picks of the Week*: Sparking Joy- concept for Marie Kondo (book and show), The Life-Changing Magic of Tidying Up by Marie Kondo; Shadowland, book by Peter Straub; The Crown, Netflix series; Catch and Kill, book by Ronan Farrow; Trick Mirror, essay collection by Jia Tolentino; Make it Stick, book by Brown, Roediger, and McDaniel
- 00:11:50 Digging into ASCVD Risk Calculator
- 00:16:12 Who should get 10 year ASCVD Risk assessment and what are the categories?
- 00:18:13 How Dr. Michos discusses healthy lifestyle and “Primordial Prevention”
- 00:19:42 What are “Risk Enhancing Factors”?
- 00:22:36 Who should get biomarker testing vs CAC scoring?
- 00:29:35 How Dr. Michos discusses statin therapy with her patients
- 00:32:18 How to address risks of side effects
- 00:37:57 Primary vs Secondary Prevention
- 00:39:40 “What should my cholesterol be?”
- 00:42:03 How often to follow-up labs?
- 00:46:00 Differences between stain intensity
- 00:47:57 How to manage side effects
- 00:52:05 PCSK9 inhibitor discussion
- 00:55:06 Aspirin, Fibrates and Icosapent Ethyl
- 01:02:13 High Risk vs Stable ASCVD
- 01:06:50 Take home points and the future
- 01:10:50 Outtro
Lipids Update – Top Pearls
- Lifestyle changes are the cornerstone and foundation of cardiovascular prevention and should never be neglected in our conversations with patients. “Primordial prevention” is key! A patient’s risk of plaque burden is not only from the magnitude of LDL elevation but duration of exposure
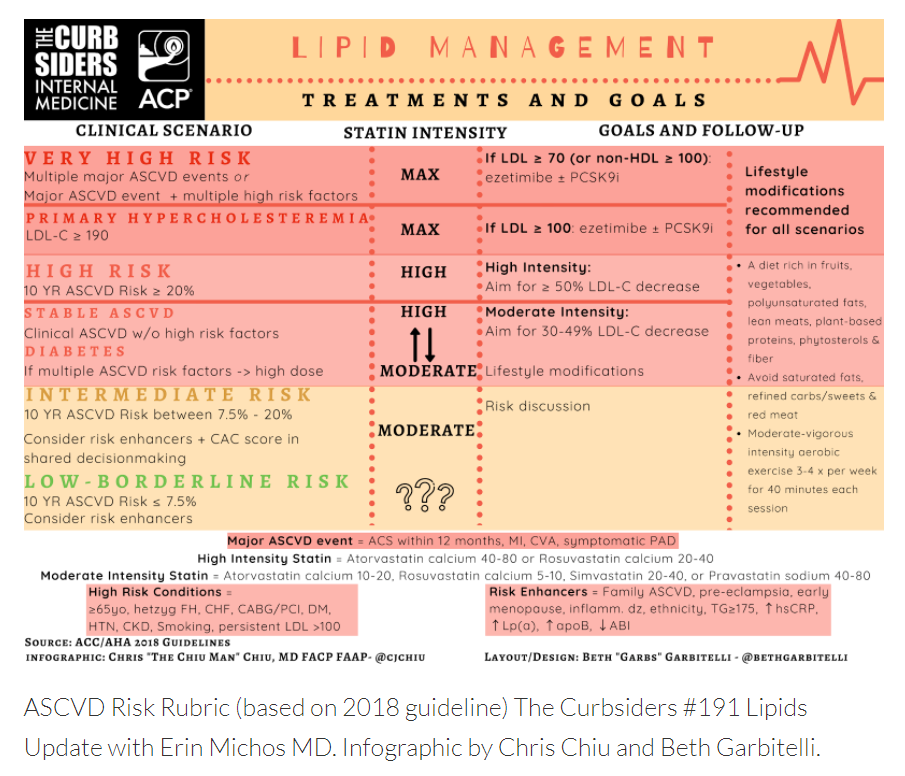
- In primary prevention, the new ASCVD risk categories include low risk (< 5%), borderline risk (5 to <7.5%), intermediate risk (7.5 to <20%), and high risk (≥20%). The focus of the 2018 lipid guideline update is on risk-enhancing factors. Use risk-enhancers (e.g. family history, chronic inflammatory disorders, pregnancy-related adverse outcomes) to guide management for patients in the borderline and intermediate risk groups
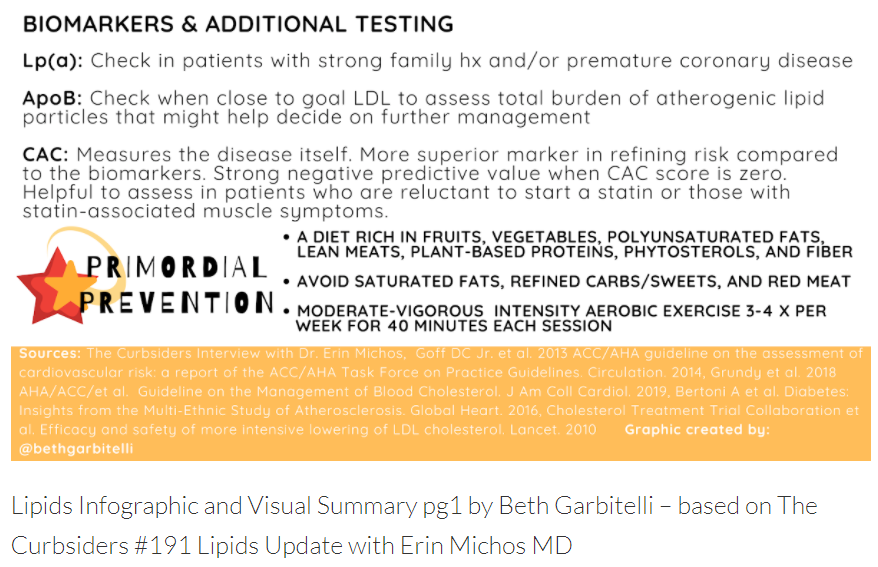
- Biomarkers that can be checked include Lp(a), ApoB, and high-sensitivity CRP, and can be helpful to further risk-stratify. Dr. Michos usually checks Lp(a) once in patients with strong family history and personal history of premature CAD. ApoB is checked when close to LDL goal to assess further need for reduction.
- Coronary artery calcium scoring is a very useful and reliable tool for the tie-breaker in starting a statin, especially in patients who are reluctant to start a statin.
- The risk of rhabdomyolysis from statins is < 0.1% and risk of liver injury is 1 in 100,000.
- Start low and go slow! Dr. Michos offers great advice in working with patients who claim to have statin “intolerance”, which the guidelines say to call “statin-associated muscle symptoms”. She recommends starting patients at a low dose and working your way up which helps with building rapport and trust from the patient.
- LDL reduction goals depend on statin intensity: with a high-intensity statin, expect an LDL reduction by > 50%, 30%-49% with moderate-intensity, and < 30% with low-intensity statin.
- For follow up, the guidelines recommend checking LDL 4-12 weeks after initiation, then 3-13 months depending on the individual patient’s situation. In stable patients, you can check yearly, and as often as every 4-6 years in younger patients.
- In secondary prevention, add ezetimibe when LDL goal has not been met, followed by PCSK9 inhibitor for further LDL reduction.
- Aspirin for primary prevention is now falling out of favor (a IIb recommendation and class III recommendation in elderly > 70). Statins and lifestyle modification are first line for patients with triglycerides > 500, however fibrates can be added when triglycerides > 1000. Icosapent ethyl is a great option, reduced major cardiovascular events by 25% in the REDUCE-IT trial, but insurance coverage may still an issue. Fish oil and icosapent ethyl are NOT the same!
Lipids Update – Show Notes
What is ASCVD risk?
Atherosclerotic Cardiovascular Disease
Atherosclerotic cardiovascular disease, or ASCVD, is defined by atherosclerotic disease such as myocardial infarction (MI), stroke, and sometimes peripheral artery disease. More specifically, this means both fatal and non-fatal MI and stroke when talking about the well-known ASCVD risk calculator.
ACC/AHA ASCVD Risk Calculator
The ASCVD risk calculator that we all know so well is one of many cardiovascular disease calculators out there, but this one is specifically recommended by the guidelines since 2013 for its use (Goff, 2013). It’s a pooled cohort equation derived from several large studies by the National Heart, Lung, and Blood Institute (NHLBI) in which the endpoints were “hard” cardiovascular endpoints, namely fatal and non-fatal MI and stroke. The calculator, which includes race, sex, presence of specific comorbidites, and other risk factors to estimate 10-year risk of these “hard” endpoints.
Kashlak Pearl: Whose risk should be assessed with this calculator? Anyone who is between the ages of 40 and 75 years-old who doesn’t have diabetes and has an LDL between 70 and 189. You got that?
Why the Update in 2018?
The guideline recommendations in 2013 encouraged widespread use of the calculator for assessing ASCVD risk and, therefore, treatment strategy with statins. But many realized that the calculator is not necessarily perfect, as it does not take into account lots of other risk enhancing factors (more below) that would put someone at a much higher risk for clinical ASCVD than what this calculator would predict. Per Dr. Michos, the 2018 update is much more personalized, and making the decision to start a statin, especially in primary prevention, is much more a patient-centered endeavor (Grundy, 2018). There is also more information in the literature on those who are “borderline” or “intermediate” risk to make a more nuanced recommendation for those who fall into these categories too.
Primary Prevention
The Foundation: Lifestyle
Dr. Michos emphasized the great importance in “primordial” prevention! This means that we start as early as possible in preventing ASCVD risk. She specifically noted that it’s not necessarily the magnitude of LDL burden but the duration of exposure that really determines ASCVD risk. Diet and exercise modification cannot be stressed enough! A life on this foundation is key for preventing ASCVD, and should be the cornerstone of our discussions with our patients at every step of the way.
A diet rich in fruits, vegetables, polyunsaturated fats, lean meats and plant-based proteins, plant phytosterols, and fiber can all potentially decrease LDL by 30 – 40 mg/dL! Avoid saturated fats, refined carbs and sweets, and red meat (Grundy, 2018). Patients should engage in moderate-to-vigorous intensity aerobic exercise about 3-4 x per week for 40 minutes each session.
Risk Categories and Recommendations
We now have 4 ASCVD risk categories per the 2018 update. These are according to the patient’s 10-year ASCVD risk:
- Low: < 5%
- Borderline: 5- <7.5%
- Intermediate: 7.5- <20%
- High: > 20%
For patients in the “intermediate” risk category, start a moderate-intensity statin based on discussion with the patient and particularly with the presence of risk-enhancing factors (class I recommendation).
For patients in the “borderline” risk category, consider a moderate-intensity statin based on patient discussion and the presence of risk-enhancing factors (class IIb recommendation).
Other Groups
Patients with diabetes mellitus and age between 40 and 75 years require at least a moderate-intensity statin (class I) or high-intensity statin (class IIa with additional risk factors) regardless of ASCVD risk.
Patients with LDL > 190 mg/dL also require a high-intensity statin regardless of ASCVD risk (class I).
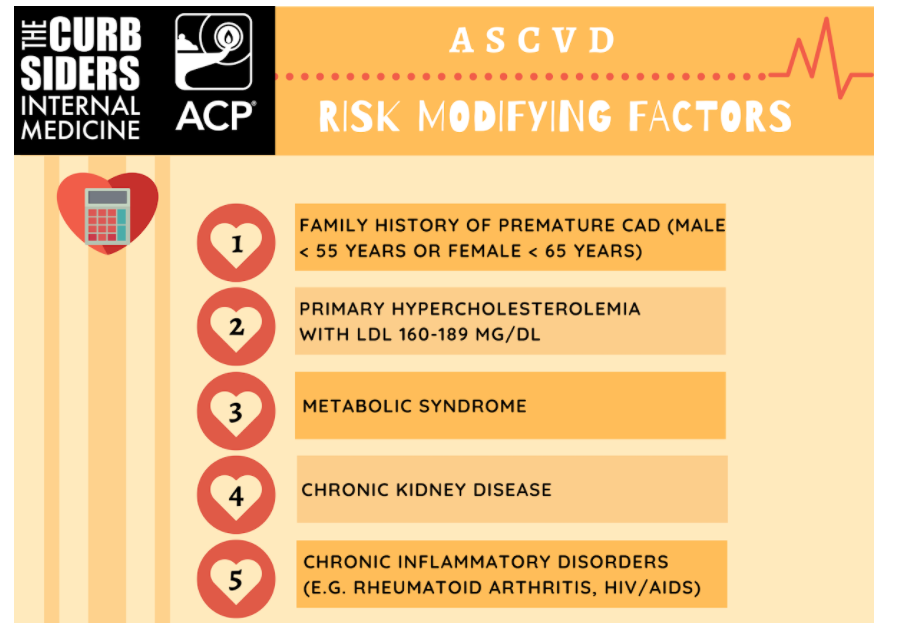
Risk Enhancing Factors
What are these risk-enhancing factors specifically? (Grundy, 2018)
- Family history of premature ASCVD (male < 55 years or female < 65 years)
- Primary hypercholesterolemia with LDL 160-189 mg/dL
- Metabolic syndrome
- Chronic kidney disease
- Chronic inflammatory disorders (e.g. rheumatoid arthritis, HIV/AIDS)
- Premature menopause (< 40 years)
- Pregnancy-associated complications with higher ASCVD risk (e.g. preeclampsia)
- High-risk ethnicities (e.g. South Asian)
- Non-fasting triglycerides > 175 mg/dL on at least 3 occasions
- Biomarkers: high-sensitivity CRP > 2 mg/dL, Lp(a) > 50 mg/dL, apoB > 130 mg/dL
- ABI < 0.9
Biomarkers
Dr. Michos usually checks lipoprotein (Lp) (a) in anyone who has a very strong family or personal history of premature CAD. Lp(a) is genetically-inherited and is worth it to check once in such patients. There might be some targeted therapies for this in the future!
She also checks an apolipoprotein B (apoB) level when she is getting close to the appropriate LDL goal. The Friedewald equation which estimates LDL levels is imperfect, and atherogenic particles are important to check to see if you need to escalate therapy.
Coronary Artery Calcium Scoring
A more accurate way to risk-stratify your patients is with coronary artery calcium (CAC) scoring, which can be particularly insightful for statin decisions in borderline or intermediate risk patients. It is a far superior marker in refining risk compared to the biomarkers themselves. It has a very strong negative predictive value with the CAC score is zero, which is equivalent to 0.1% per year risk of ASCVD. According to the MESA study (Bertoni, 2016), diabetics with a CAC score of zero had similar event rate as those without diabetes.
The guidelines highlight some select groups of people that CAC scoring could benefit (Grundy, 2018):
- Patients who are reluctant to start a statin
- Patients who are reluctant to re-start a statin after stopping for statin-associated symptoms
- Older patients (men 50-88 years and women 60-80 years) with low burden of risk factors and question benefit of starting a statin
- Middle-aged adults (40-55 years) who fall in the “borderline” ASCVD risk category and have additional risk factors that increase their ASCVD risk
Secondary Prevention
Secondary prevention is prevention of further ASCVD after a clinical event (like myocardial infarction, stroke, peripheral arterial or coronary revascularization) has occurred, and is a little less complicated. The two main groups in secondary prevention are “high risk” ASCVD and “stable” ASCVD. These people always get a high intensity statin right off the bat (unless the patient is > 75 years-old in which case it is a IIa recommendation to start moderate or high intensity statin).
It is about LDL goals for these people: do they achieve LDL < 70 mg/dL on a high intensity statin? If yes, then that’s awesome! If not, then we have to start thinking about adherence conversations and other medications.
Ezetimibe and PCSK9 Inhibitors
When thinking of additional medications to add to a statin for further lipid lowering events, think no further than ezetimibe and PCSK9 inhibitors! The IMPROVE-IT, as well as ODYSSEY and FOURIER trials really showed us the added benefits of ezetimibe and PCSK9 inhibitors, respectively. IMPROVE-IT showed that the addition of ezetimibe to moderate-intensity statin reduced cardiovascular mortality, major cardiovascular events overall, and ischemic stroke (Cannon, 2015). Moreover, PCSK9 inhibitors showed benefit when added to high intensity statin in patients with known coronary disease or familial hypercholesterolemia in the ODYSSEY trial (Robinson, 2015). There was a 62% reduction in LDL in these patients with no increase in cardiovascular events, and a post-hoc analysis showed a 2% absolute risk reduction in major cardiovascular events (MACE). The FOURIER trial also showed 1.5% absolute reduction in MACE when added to a high intensity statin with LDL above 70 mg/dL (Sabatine, 2017).
High Risk ASCVD
Patients deemed as being in the “high risk” ASCVD group are those with the following:
- Acute coronary syndrome (ACS) in the last 12 months
- Multiple heart attacks
- Ischemic stroke
- Symptomatic peripheral artery disease (claudication with ABI < 0.85, or previous revascularization or amputation)
- Age > 65 years
- Heterozygous familial hypercholesterolemia*
- Prior coronary bypass surgery or PCI outside of the above events
- Diabetes mellitus
- Hypertension
- Chronic kidney disease
- Current smoker
- Persistently elevated LDL > 100 mg/dL despite max statin therapy and ezetimibe
- Congestive heart failure
These patients at “high risk” of future events require maximum-tolerated high intensity statin (Class I indication). It is a class IIa recommendation to add on ezetimibe if LDL > 70 mg/dL while already on a high intensity statin. A PCSK9 inhibitor can be considered either after trying a high intensity statin and ezetimibe and the LDL is still > 70 mg/dL (class I), or one can consider it after “clinically judged maximal LDL-lowering therapy” (class IIa).
*Please see:
- Familial Hypercholesterolemia: Early Diagnosis and Treatment is Key for Cardiovascular Prevention, Apr 16, 2020 | Nishant Shah, MD, FACC Expert Analysis, from American College of Cardiology Latest In Cardiology.
- Defining severe familial hypercholesterolaemia and the implications for clinical management: a consensus statement from the International Atherosclerosis Society Severe Familial Hypercholesterolemia Panel [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Lancet Diabetes Endocrinol. 2016 Oct;4(10):850-61.
Stable ASCVD
Patients who have established coronary disease but do not meet any of the “high risk” categories listed above fall into this group. If the patient is > 75 years old, as noted above, it is a class IIb recommendation to start either a moderate or high intensity statin. If the patient is < 75 years old, they get a high intensity statin with a goal of LDL < 70 mg/dL, or moderate intensity statin if they cannot tolerate it (Class I). If the LDL does not drop below 70 mg/dL…you guessed it! Add ezetimibe!
Follow Up and Goals
The earliest you should recheck a lipid panel after starting a statin is at 4-12 weeks (1-3 months). Afterwards, you can check anywhere from 3 to 13 months depending on the patient and their situation.
You goals are going to depend on the ASCVD risk category of your patient in primary prevention. For those in the “intermediate” category, an LDL reduction of 30-49% is appropriate. In those at high risk, however, require a reduction of LDL by > 50%. Anyone who does not meet these goals can be considered for step up in therapy.
For our secondary prevention group, you know the magic number: get that LDL < 70 mg/dL!
Is there a difference between, say for example, atorvastatin 80 mg and 40 mg? Well, yes there is! Expect to see a 50-60% reduction of LDL with atorvastatin 80 mg, and 40-52% reduction with the 40 mg.
There is no floor for LDL! The lower you can go, the better. There is no such thing as an LDL that is “too low”.
Misconceptions and Misinformation
“Side-effect” or “intolerance”? I think not! The guidelines recommend avoiding these terms and calling the patients’ symptoms “statin-associated muscle symptoms”. This helps to encourage reframing and redefining their symptoms without dismissing them.
Although there is a high concern for major side effects amongst popular thought, the risk of severe muscle injury or rhabdomyolysis from a statin is < 0.1%, and the risk of drug-induced liver injury is 1 in 10.0,000 (Cholesterol Treatment Trialists, 2010, Thapar 2013)! Additionally, there is no evidence for certain side-effects, namely cataracts and cognitive decline per large randomized trials. There are lots of safety data out there, which is helpful in your discussions with your patients.
Statin-Associated Muscle Symptoms
Many patients will tell us they have myalgias after the initiation of a statin, and many will defer taking it altogether due to concerns for severe muscle damage as a side-effect. In fact, only up to 10% of patients will develop Myalgias without CK elevation; Myalgies with CK elevation, rhabdomyolysis and statin associated autoimmune myopathy are RARE (Grundy, 2018, see Table 11)! Some studies have shown that patients with previous statin intolerance were able to tolerate statins when rechallenged, up to 72.5% (Warner 2013).
How To Discuss Starting (Or Restarting) a Statin
DISCUSS THE OVERARCHING BENEFITS
Start by discussing the benefits. We know that for every 1 mmol/L, or 39 mg/dL of LDL reduction, the relative risk reduction of cardiovascular events is 22% (Silverman, 2016). There is also even a 10% reduction in mortality! Moreover, those who have higher risk reap even more benefit. Share the data with the patient; numbers are tangible and meaningful.
DISCUSS THE PATIENT’S PERSONAL BENEFIT
Now hone in on the personal benefits. After sharing the science above, personalize it. Show them what these numbers mean to your patients, especially with their specific ASCVD risk.
ADDRESS THE SAMS
Statin-associated muscle symptoms can be a big concern for patients when starting or restarting a statin. It’s all about building trust and working with your patient. For the statin-naive, discuss the numbers and personalize it, as well as possible. For instance, utilizing CAC scoring if relevant can help further this discussion in a positive way. For those who have already experienced SAMS, avoid dismissing them and discuss re-introducing the statin. Dr. Michos recommends to start low and go slow. We can start at a low dose statin and slowly work your way up. Chances are, your patient will not have those SAMs anymore (see evidence from randomized trials above). For the most reluctant patients, Dr. Michos will do rosuvastatin 5 mg every other day with ezetimibe. Keep in mind, simvastatin and lovastatin tend to have more SAMS. Pravastatin tends to be less effective.
What’s The Deal With Aspirin? Aspirin and More
The Scoop on Aspirin
Start here.