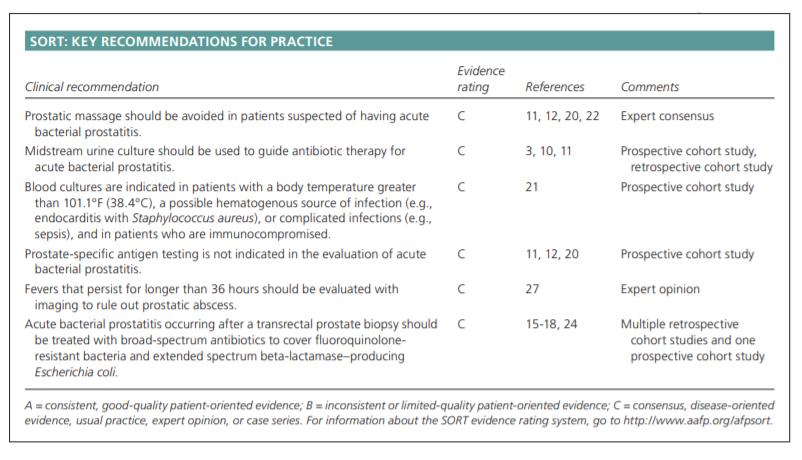
In this post I link to and excerpt from Acute Bacterial Prostatitis: Diagnosis and Management [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. TIMOTHY J. COKER, MD, and DANIEL M. DIERFELDT, DO, Ehrling Bergquist Family Medicine Residency Program, Offutt Air Force Base, Nebraska. Am Fam Physician. 2016 Jan 15;93(2):114-120.
All that follows is from the above resource.
Patient information: A handout on this topic is available at https://familydoctor.org/familydoctor/en/diseases-conditions/prostatitis.html.
Abstract
Acute bacterial prostatitis is an acute infection of the prostate gland that causes pelvic pain and urinary tract symptoms, such as dysuria, urinary frequency, and urinary retention, and may lead to systemic symptoms, such as fevers, chills, nausea, emesis, and malaise. Although the true incidence is unknown, acute bacterial prostatitis is estimated to comprise approximately 10% of all cases of prostatitis. Most acute bacterial prostatitis infections are community acquired, but some occur after transurethral manipulation procedures, such as urethral catheterization and cystoscopy, or after transrectal prostate biopsy. The physical examination should include abdominal, genital, and digital rectal examination to assess for a tender, enlarged, or boggy prostate. Diagnosis is predominantly made based on history and physical examination, but may be aided by urinalysis. Urine cultures should be obtained in all patients who are suspected of having acute bacterial prostatitis to determine the responsible bacteria and its antibiotic sensitivity pattern. Additional laboratory studies can be obtained based on risk factors and severity of illness. Radiography is typically unnecessary. Most patients can be treated as outpatients with oral antibiotics and supportive measures. Hospitalization and broad-spectrum intravenous antibiotics should be considered in patients who are systemically ill, unable to voluntarily urinate, unable to tolerate oral intake, or have risk factors for antibiotic resistance. Typical antibiotic regimens include ceftriaxone and doxycycline, ciprofloxacin, and piperacillin/tazobactam. The risk of nosocomial bacterial prostatitis can be reduced by using antibiotics, such as ciprofloxacin, before transrectal prostate biopsy.
Introduction
Acute bacterial prostatitis is an acute infection of the prostate gland that causes urinary tract symptoms and pelvic pain in men.1 It is estimated to comprise up to 10% of all prostatitis diagnoses, and its incidence peaks in persons 20 to 40 years of age and in persons older than 70 years.2 Most cases can be diagnosed with a convincing history and physical examination.3 Although prostatitis-like symptoms have a combined prevalence of 8.2% in men, the incidence and prevalence of acute bacterial prostatitis are unknown.4
Pathogenesis
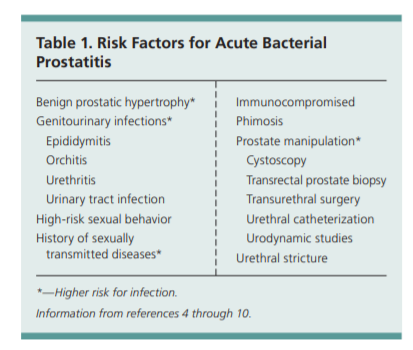
Most cases of acute bacterial prostatitis are caused by ascending urethral infection or intraprostatic reflux and are facilitated by
numerous risk factors (Table 1).4-10Microbiology
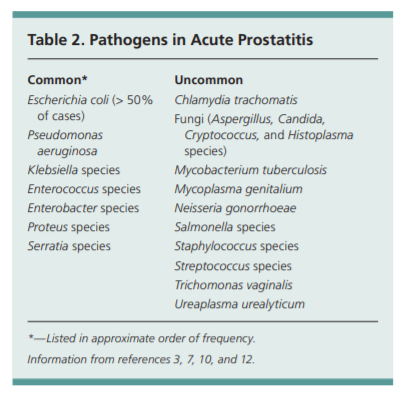
Acute bacterial prostatitis is most frequently
caused by Escherichia coli, followed by Pseudomonas aeruginosa, and Klebsiella, Enterococcus, Enterobacter, Proteus, and Serratia species.3,5,7,10 In sexually active men, Neisseria gonorrhoeae and Chlamydia trachomatis should be considered.12 Patients who areimmunocompromised (e.g., persons withhuman immunodeficiency virus) are more
likely to have uncommon causes for prostatitis, such as Salmonella, Candida, and Cryptococcus species (Table 2).
3,7,10,12Clinical Presentation
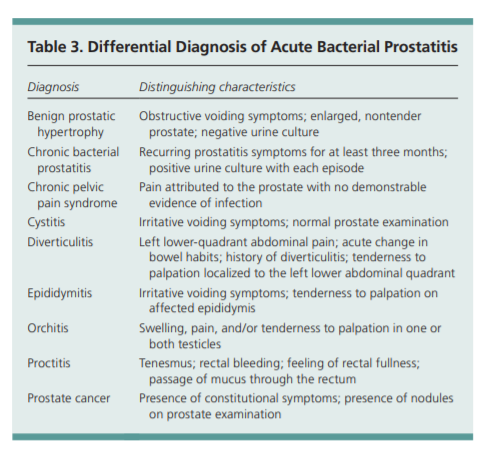
Patients with acute bacterial prostatitis often present
with acute onset of irritative (e.g., dysuria, urinary frequency, urinary urgency) or obstructive (e.g., hesitancy,
incomplete voiding, straining to urinate, weak stream)
voiding symptoms. Patients may report suprapubic, rectal, or perineal pain.6,9,11 Painful ejaculation, hematospermia, and painful defecation may be present as well.19 Systemic symptoms, such as fever, chills, nausea, emesis, and malaise, commonly occur, and their presence should prompt physicians to determine if patients meet clinical criteria for sepsis.The physical examination should include an abdominal examination to detect a distended bladder and costovertebral angle tenderness, a genital examination, and a
digital rectal examination. A digital rectal examination
should be performed gently because vigorous prostatic
massage can induce bacteremia, and subsequently, sepsis.9,11,20 In a patient with acute bacterial prostatitis, the
prostate will often be tender, enlarged, or boggy. If there
is concern for obstructed voiding, postvoid residual urine
volumes should be measured using ultrasonography.Several conditions present with similar symptoms and must be differentiated from acute bacterial prostatitis (Table 3).
Evaluation
Blood cultures should be collected before initiating antibiotics in patients with a body temperature greater than 101.1°F (38.4°C),
a possible hematogenous source of infection (e.g., endocarditis with Staphylococcus aureus), complicated infections (e.g., sepsis), or who are immunocompromised.11,21 Although blood and urine cultures can aid in diagnosis and management, up to 35% of urine cultures in patients with acute prostatitis will fail to grow an organism.3In men younger than 35 years who are sexually active,
and in men older than 35 years who engage in high-risk
sexual behavior, a Gram stain of urethral swabs, a culture of urethral discharge, or a DNA amplification test should be obtained to evaluate for N. gonorrhoeae and C. trachomatis. 11,22Urine testing before and after prostatic massage (also
known as the Meares-Stamey 2-glass or 4-glass test) is
useful in diagnosing chronic prostate and pelvic disorders; however, such testing should not be performed
in patients with suspected acute bacterial prostatitis
because prostatic massage increases the risk of bacteremia, and subsequently, sepsis.Prostate-specific antigen (PSA) levels are not indicated
in the workup of acute bacterial prostatitis.11,12,20 Approximately 70% of men will have a spurious PSA elevation
due to disruption of prostatic architecture caused by
inflammation.19 Elevated PSA levels can persist for one to
two months after treatment.11,12 If PSA levels remain elevated for more than two months, prostate cancer should
be considered because 20% of persistent elevations are
associated with malignancy.19IMAGING
Imaging studies are usually unnecessary during the initial evaluation, but may help when the diagnosis remains
unclear or when patients do not respond to adequate
antibiotic therapy. Patients who remain febrile after 36
hours or whose symptoms do not improve with antibiotics
should undergo transrectal ultrasonography to evaluate
for prostatic abscess. Alternatively, noncontrast computed
tomography (CT) or magnetic resonance imaging (MRI)
of the pelvis could be considered. Prostate biopsy should
not be performed to avoid inducing septicemia.Management
Management of acute bacterial prostatitis should be
based on severity of symptoms, risk factors, and local
antibiotic resistance patterns (Figure 1).Most patients can be treated with outpatient antibiotics; fewer than one in six patients will require hospitalization.6
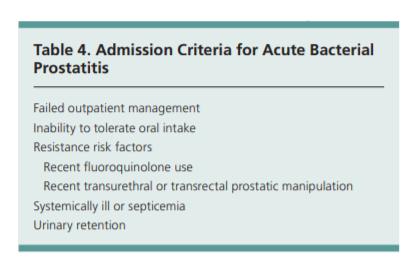
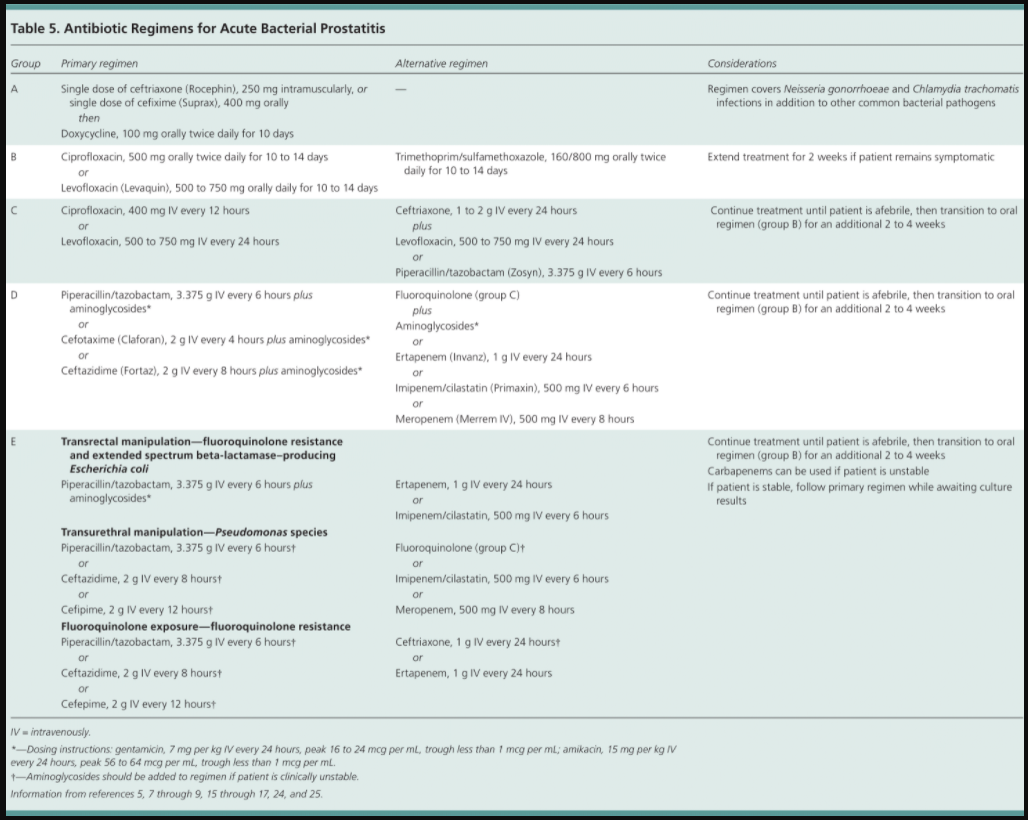
Admission criteria are listed in Table 4.Initial empiric antibiotic therapy should be based on the suspected mode of infection and the presumed infecting organism (Table 5).5,7-9,15-17,24,25
Antibiotics should be adjusted based on culture and sensitivity results, when available.10,15 Men younger than 35 years who are sexually active and men older than 35 years who engage in high-risk sexual behavior should be treated with regimens that cover N. gonorrhoeae and C. trachomatis. 12 Patients with risk factors for antibiotic resistance require intravenous therapy with broad-spectrum regimens because of the high likelihood of complications.7,8,15,24
Complications
Prostatic abscesses occur in 2.7% of patients with acute
bacterial prostatitis and require urology consultation for
drainage.6 Risk factors for prostatic abscess include longterm urinary catheterization, recent urethral manipulation, and an immunocompromised state.Approximately 13% of patients with acute bacterial
prostatitis experience recurrence necessitating a longer course of antibiotics.6 Patients with persistent or recurrent symptoms should have a repeat urine culture to evaluate for repeat bacterial prostatitis and be treated based on culture results.After three months of persistent or recurrent symptoms, patients should be evaluated and treated based on chronic prostate syndrome guidelines.1 Approximately one in nine patients with acute bacterial prostatitis will develop chronic bacterial prostatitis or chronic pelvic pain syndrome.29