This post contains links to and excerpts from Coronary Microvascular Function and Cardiovascular Risk Factors in Women With Angina Pectoris and No Obstructive Coronary Artery Disease: The iPOWER Study [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Heart Assoc. 2016 Mar 15;5(3):e003064. doi: 10.1161/JAHA.115.003064.
The above article has been cited by 15 PubMed Central articles.
Here are excerpts from the above article:
Background-—The majority of women with angina-like chest pain have no obstructive coronary artery disease when evaluated with coronary angiography. Coronary microvascular dysfunction is a possible explanation and associated with a poor prognosis. This study evaluated the prevalence of coronary microvascular dysfunction and the association with symptoms, cardiovascular risk factors, psychosocial factors, and results from diagnostic stress testing.
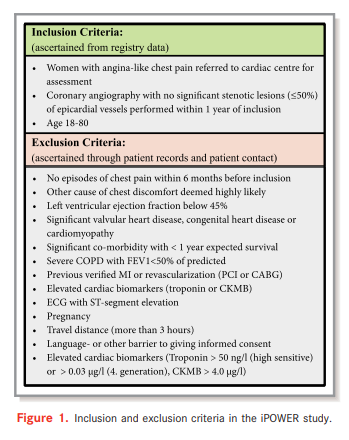
Methods and Results-—After screening 3568 women, 963 women with angina-like chest pain and a diagnostic coronary
angiogram without significant coronary artery stenosis (<50%) were consecutively included. Mean age (SD) was 62.1 (9.7).
Assessment included demographic and clinical data, blood samples, questionnaires, and transthoracic echocardiography during rest and high-dose dipyridamole (0.84 mg/kg) with measurement of coronary flow velocity reserve (CFVR) by Doppler examination of the left anterior descending coronary artery. CFVR was successfully measured in 919 (95%) women. Median (IQR) CFVR was 2.33 (1.98–2.76), and 241 (26%) had markedly impaired CFVR (<2). In multivariable regression analysis, predictors of impaired CFVR were age (P<0.01), hypertension (P=0.02), current smoking (P<0.01), elevated heart rate (P<0.01), and low high-density lipoprotein cholesterol (P=0.02), but these variables explained only a little of the CFVR variation (r²=0.09). CFVR was not associated with chest pain characteristics or results from diagnostic stress testing.Conclusion-—Impaired CFVR was detected in a substantial proportion, which suggests that coronary microvascular dysfunction
plays a role in the development of angina pectoris. CFVR was associated with few cardiovascular risk factors, suggesting that CFVR is an independent parameter in the risk evaluation of these women. Symptom characteristics and results from stress testing did not identify individuals with impaired CFVR.
We found that 26% of the women had CFVR <2 and, thus,
CMD according to current guidelines.17 This is in agreement
with several other studies.It is often assumed that a positive stress test in the
presence of no obstructive CAD is indicative of microvascular
dysfunction. One study of 68 women found that significantly
more women with low CFVR had a positive clinical stress
test.21 This could not be corroborated in our study: among the
47% of participants who had a stress test performed, a
positive stress test was not predictive of CMD. A recent large
study that included 1439 subjects with angina and invasive
assessment of CMD also found no association between
results of stress testing and CMD.23 The cause of the positive
stress tests is unclear; however, it is plausible that CMD can
cause ischemia without positive stress testing since these are
mostly based on demonstration of regional rather than diffuse
ischemia.
I wonder if the above lack of correlation between a positive stress test and coronary micro vascular dysfunction noted above might be explained by the author’s following observation:
We have assessed 1 dimension of CMD; the adenosineinduced reduced CFVR, which is mainly caused by dysfunction
of the endothelium-independent vasodilation of the microcirculation. We have not assessed the endothelium-dependent epicardial dysfunction or microvascular spasm, which can be detected by using invasive acetylcholine provocation test.32–34 The latter might have been the main mechanism responsible for chest pain in a subgroup of participants included in this study, in particular those with unstable angina pectoris. Therefore, the burden of CMD might be underestimated in this study.