This post contains links to and excerpts from How to Diagnose and Manage Angina Without Obstructive Coronary Artery Disease: Lessons from the British Heart Foundation CorMicA Trial [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Interv Cardiol. 2019 May 21;14(2):76-82. doi: 10.15420/icr.2019.04.R1. eCollection 2019 May.
Here are excerpts from the above article:
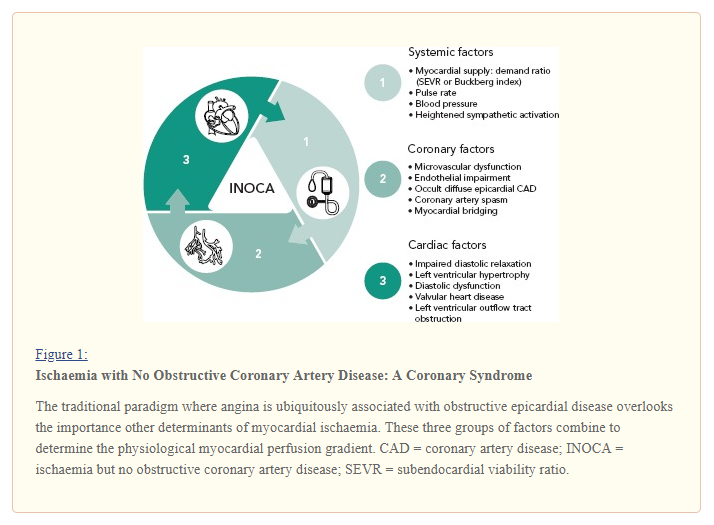
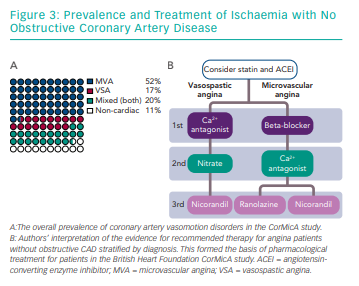
Invasive coronary angiography is the reference test for angina and identifies obstructive coronary artery disease (CAD) as a cause for symptoms. In Europe and the US, approximately 4 million elective coronary angiograms are performed each year.2,3 However, up to half of all angina patients undergoing elective coronary angiography with symptoms and/or signs of ischaemia have no obstructive epicardial coronary artery disease (INOCA).3 This large, heterogeneous group includes patients with microvascular angina (MVA), vasospastic angina (VSA) or both conditions together. The burden of these conditions on physical and mental wellbeing can be profound; they are associated with morbidity4 and a reduction in quality of life.5 Patients with these conditions commonly attend primary and secondary care, driving up health resource utilisation.6
Depending on the patient population studied and the techniques
used, between one-third and two-thirds of angina patients with a negative angiogram have an underlying disorder of coronary vascular function.8,9 Importantly, the two most common causes of INOCA (MVA and VSA) are not excluded by a negative non-invasive CT coronary angiogram or invasive coronary angiogram.6 For affected patients, symptom burden, morbidity and health resource utilisation can be considerable.5,10,11
The authors of this study argue that non-invasive evaluation of ischemic nonobstructive coronary artery disease (INOCA) is inadequate and they state that an interventional diagnostic procedure (IDP) can better characterize the mechanism of INOCA in individual patients.
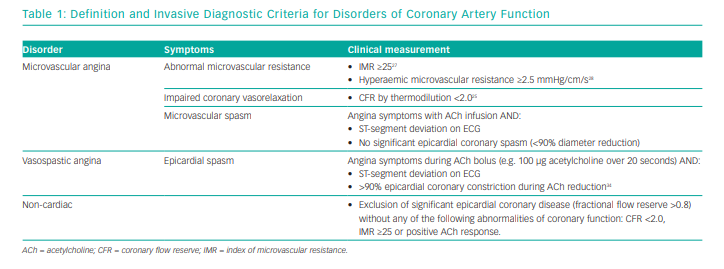
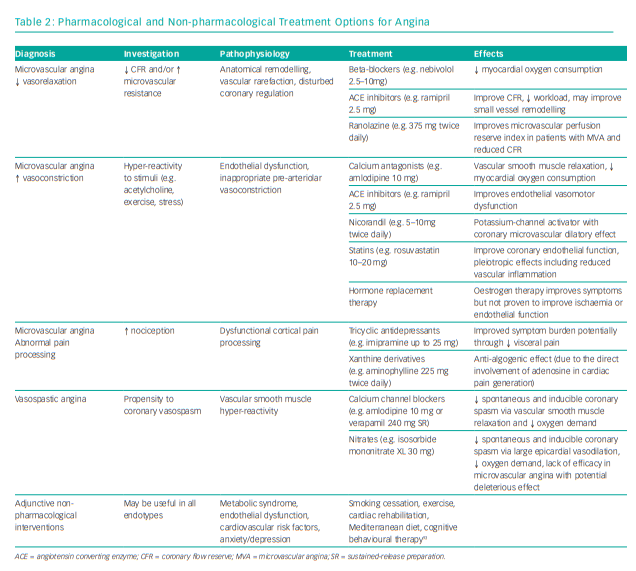
The IDP consists of two steps: assessment of coronary circulation vasorelaxation using invasive coronary physiology at rest and with hyperaemia; and second, assessment of the propensity of the coronary circulation to excessive vasoconstriction using intra-arterial acetylcholine (microvascular and/or epicardial vasospasm) (Table 1).
We typically prefer the left anterior descending coronary artery as the target vessel because it subtends the largest myocardial mass. While regional microvascular dysfunction is well recognised, interrogation of multiple vessels increases the procedural duration such that the benefits of testing may be outweighed by the risks.
text
text
text