In this post I link to and excerpt from Free, brief, and validated: Standardized instruments for low-resource mental health settings [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Cogn Behav Pract. 2015 Feb 1;22(1):5-19
The above article has been cited by 22 articles in the PubMed Archives.
Here is a list of 52 articles that are similar to the above article in PubMed Archives.
All that follows are excerpts from the above article.
Abstract
Evidence-based assessment [EBA] has received little attention despite its critical importance to the evidence-based practice [EBP] movement. Given the limited resources in the public sector, it is necessary for evidence-based assessment to utilize tools with established reliability and validity metrics that are free, easily accessible, and brief. We review tools that meet these criteria for youth and adult mental health for the most prevalent mental health disorders to provide a clinical guide and reference for the selection of assessment tools for public sector settings. We also discuss recommendations for how to move forward the evidence-based assessment agenda.
_____________________________________________
Evidence-Based Assessment [EBA] is critical to effective Evidence-Based Practice [EBP].
Therefore, EBA is critical to any evidence-based treatment approach. Given the importance of EBA, to date, two special issues of peer-reviewed journals have focused on EBA in both adult and youth populations: see special issues of Psychological Assessment (Hunsley & Mash, 2005) and the Journal of Clinical Child and Adolescent Psychology (Mash & Hunsley, 2005). These special issues have resulted in recommendations on EBA for a variety of disorders, including youth and adult anxiety (Antony & Rowa, 2005; Silverman & Ollendick, 2005), adult depression (Joiner, Walker, Pettit, Perez, & Cukrowicz, 2005), youth disruptive behavior disorders (McMahon & Frick, 2005), and youth bipolar disorder (Youngstrom, Findling, Kogos-Youngstrom, & Calabrese, 2005).
Although these reviews have resulted in important recognition of the importance of EBA and preliminary guidelines, they have not always been as applicable to low resource mental health settings such as those in the public sector because they have featured resource-intensive ways to engage in EBA. In the pages that follow, we identify and address issues related to the use of standardized tools in low resource mental health settings.
Given the known barriers to implementation of EBPs in community settings and our desire to increase EBA in the public sector, assessments must be brief, free or low cost, validated for use in multiple populations particularly ethnic minority and low socioeconomic status individuals, and straightforward and brief to administer, score and interpret (Jensen-Doss & Hawley, 2010). These recommendations are echoed by public health researchers who recommend that for standardized assessment instruments to be usable, they must be important to stakeholders in addition to researchers, low burden to administer, broadly applicable, sensitive to change, and represent constructs that are actionable (i.e., clinician or patient can do something about them; Glasgow & Riley, 2013).
Accordingly, the goal of this paper is to conduct a review of EBA instruments for the most prevalent mental health disorders in youths and adults that meet the criteria delineated above. We focus on instruments that can be used for screening (i.e., identifying those at risk for a disorder), diagnosis (i.e., identifying those who meet DSM criteria), and/or treatment monitoring and evaluation (i.e., evaluating the success of treatment or interim response to treatment (Hunsley & Mash, 2008). We hope this manuscript can serve as a clinical guide and reference for the selection of assessment instruments for low-resource mental health settings.
Inclusion and Exclusion Criteria
We utilized the following criteria when deciding whether or not to include measures: we required that the measures be free, easily accessible via the Internet or the author of the measure, brief (items < 50), have established reliability and validity, and be relevant for the most prevalent mental health disorders (e.g., anxiety, depression, trauma-associated disorders, oppositional behavior disorders; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Merikangas et al., 2010). We crafted these criteria based on a recent paper written by Glasgow & Riley (2013) encouraging the use of pragmatic measures.
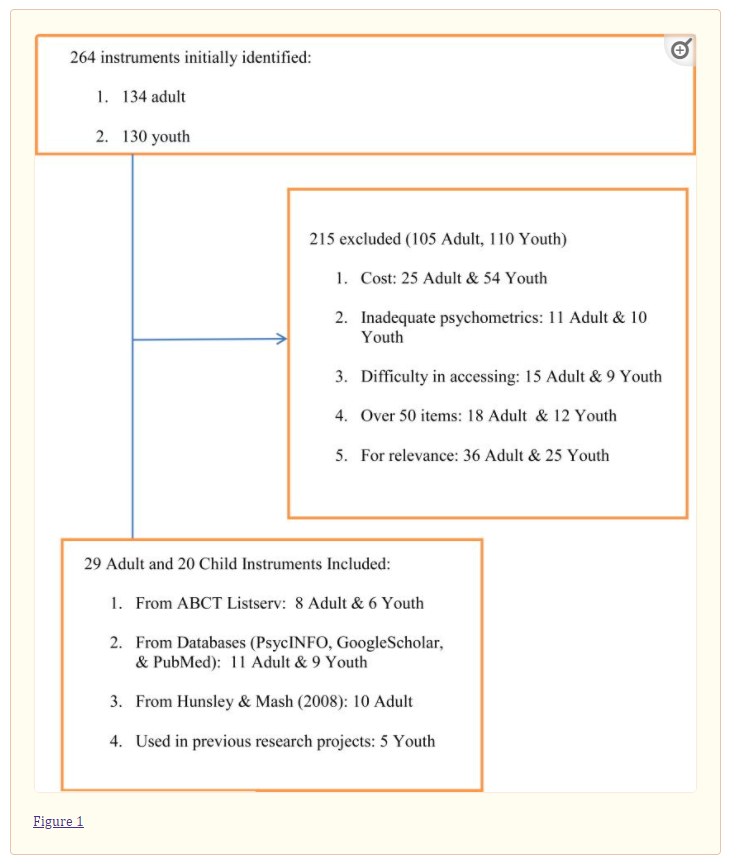
See Figure 1 for the number of instruments that were identified, reviewed, included, and excluded.
Instrument Classification
Given that instruments can serve multiple purposes (i.e., diagnosis, screening, and treatment monitoring/evaluation), we elected to classify the manner in which each instrument could be used. Instruments may be used for: (a) diagnosis: to determine “the nature and/or cause of the presenting problem”; (b) screening: to identify “those who are at risk…or who might be helped by further assessment or intervention”; and/or (c) treatment monitoring and evaluation: “track changes in symptoms and functioning” or determine “effectiveness…of the intervention.”(p. 6, Hunsley & Mash, 2008). An instrument could be designated as meeting all three criteria.
We operationally defined instruments as appropriate for diagnosis if they were created to map on to DSM criteria.
Instruments met criteria for screening if the questions queried for symptoms of a mental health disorder or behavioral and/or emotional difficulties.
Finally, instruments were classified as treatment monitoring and evaluation instruments if they could be used for screening or diagnosis, and data were available on the instrument’s sensitivity to change following psychotherapy or psychotropic medication.
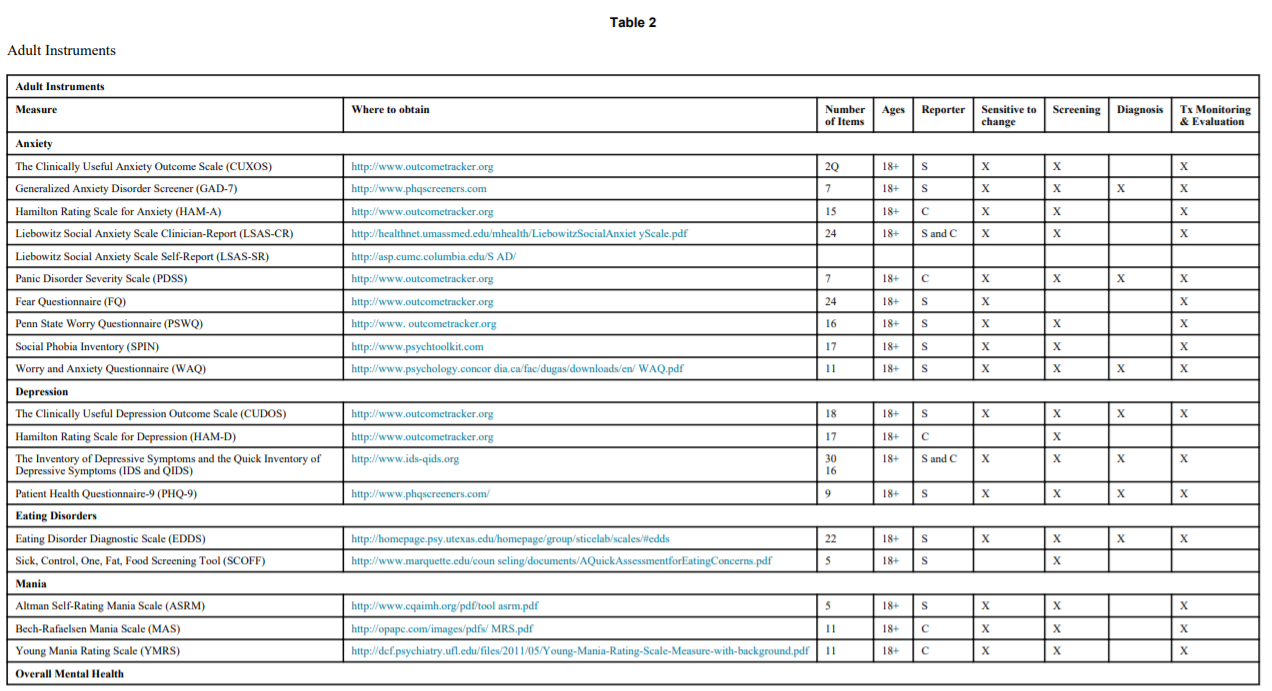
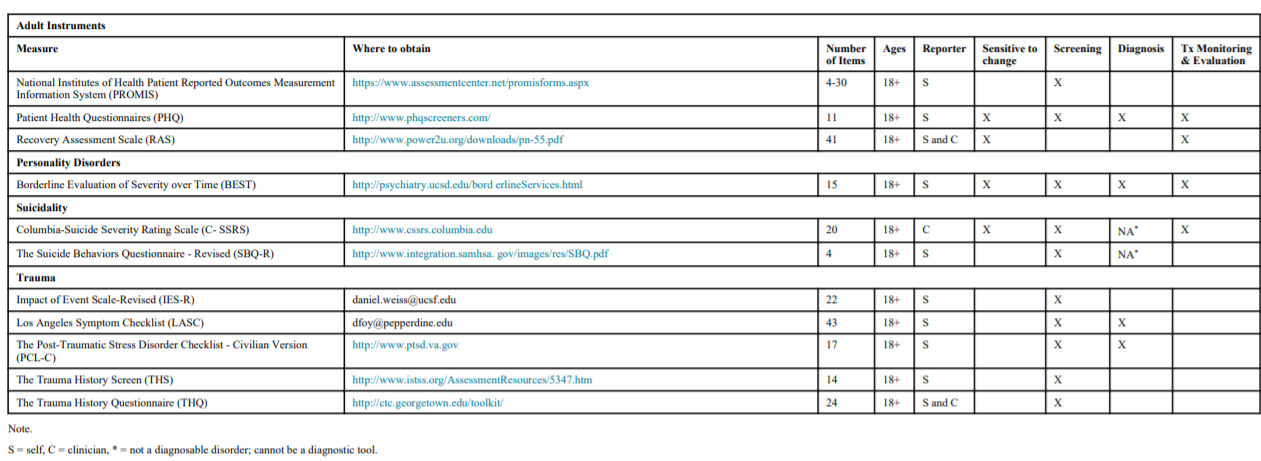
Table 2
Adult Instruments
Adult Instruments Measure Where to obtain Number
of ItemsAges Reporter Sensitive to
changeScreening Diagnosis Tx Monitoring
& EvaluationAnxiety The Clinically Useful Anxiety Outcome Scale (CUXOS) http://www.outcometracker.org 2Q 18+ S X X X Generalized Anxiety Disorder Screener (GAD-7) http://www.phqscreeners.com 7 18+ S X X X X Hamilton Rating Scale for Anxiety (HAM-A) http://www.outcometracker.org 15 18+ C X X X Liebowitz Social Anxiety Scale Clinician-Report (LSAS-CR) http://healthnet.umassmed.edu/mhealth/LiebowitzSocialAnxiet yScale.pdf 24 18+ S and C X X X Liebowitz Social Anxiety Scale Self-Report (LSAS-SR) http://asp.cumc.columbia.edu/S AD/ Panic Disorder Severity Scale (PDSS) http://www.outcometracker.org 7 18+ C X X X X Fear Questionnaire (FQ) http://www.outcometracker.org 24 18+ S X X Penn State Worry Questionnaire (PSWQ) http://www. outcometracker.org 16 18+ S X X X Social Phobia Inventory (SPIN) http://www.psychtoolkit.com 17 18+ S X X X Worry and Anxiety Questionnaire (WAQ) http://www.psychology.concor dia.ca/fac/dugas/downloads/en/ WAQ.pdf 11 18+ S X X X X Depression The Clinically Useful Depression Outcome Scale (CUDOS) http://www.outcometracker.org 18 18+ S X X X X Hamilton Rating Scale for Depression (HAM-D) http://www.outcometracker.org 17 18+ C X The Inventory of Depressive Symptoms and the Quick Inventory of Depressive Symptoms (IDS and QIDS) http://www.ids-qids.org 30
1618+ S and C X X X X Patient Health Questionnaire-9 (PHQ-9) http://www.phqscreeners.com/ 9 18+ S X X X X Eating Disorders Eating Disorder Diagnostic Scale (EDDS) http://homepage.psy.utexas.edu/homepage/group/sticelab/scales/#edds 22 18+ S X X X X Sick, Control, One, Fat, Food Screening Tool (SCOFF) http://www.marquette.edu/coun seling/documents/AQuickAssessmentforEatingConcerns.pdf 5 18+ S X Mania Altman Self-Rating Mania Scale (ASRM) http://www.cqaimh.org/pdf/tool asrm.pdf 5 18+ S X X X Bech-Rafaelsen Mania Scale (MAS) http://opapc.com/images/pdfs/ MRS.pdf 11 18+ C X X X Young Mania Rating Scale (YMRS) http://dcf.psychiatry.ufl.edu/files/2011/05/Young-Mania-Rating-Scale-Measure-with-background.pdf 11 18+ C X X X Overall Mental Health National Institutes of Health Patient Reported Outcomes Measurement Information System (PROMIS) https://www.assessmentcenter.net/promisforms.aspx 4-30 18+ S X Patient Health Questionnaires (PHQ) http://www.phqscreeners.com/ 11 18+ S X X X X Recovery Assessment Scale (RAS) http://www.power2u.org/downloads/pn-55.pdf 41 18+ S and C X X Personality Disorders Borderline Evaluation of Severity over Time (BEST) http://psychiatry.ucsd.edu/bord erlineServices.html 15 18+ S X X X X Suicidality Columbia-Suicide Severity Rating Scale (C- SSRS) http://www.cssrs.columbia.edu 20 18+ C X X NA* X The Suicide Behaviors Questionnaire – Revised (SBQ-R) http://www.integration.samhsa. gov/images/res/SBQ.pdf 4 18+ S X NA* Trauma Impact of Event Scale-Revised (IES-R) ude.fscu@ssiew.leinad 22 18+ S X Los Angeles Symptom Checklist (LASC) ude.enidreppep@yofd 43 18+ S X X The Post-Traumatic Stress Disorder Checklist – Civilian Version (PCL-C) http://www.ptsd.va.gov 17 18+ S X X The Trauma History Screen (THS) http://www.istss.org/AssessmentResources/5347.htm 14 18+ S X The Trauma History Questionnaire (THQ) http://ctc.georgetown.edu/toolkit/ 24 18+ S and C X Note.
S = self, C = clinician, * = not a diagnosable disorder; cannot be a diagnostic tool.
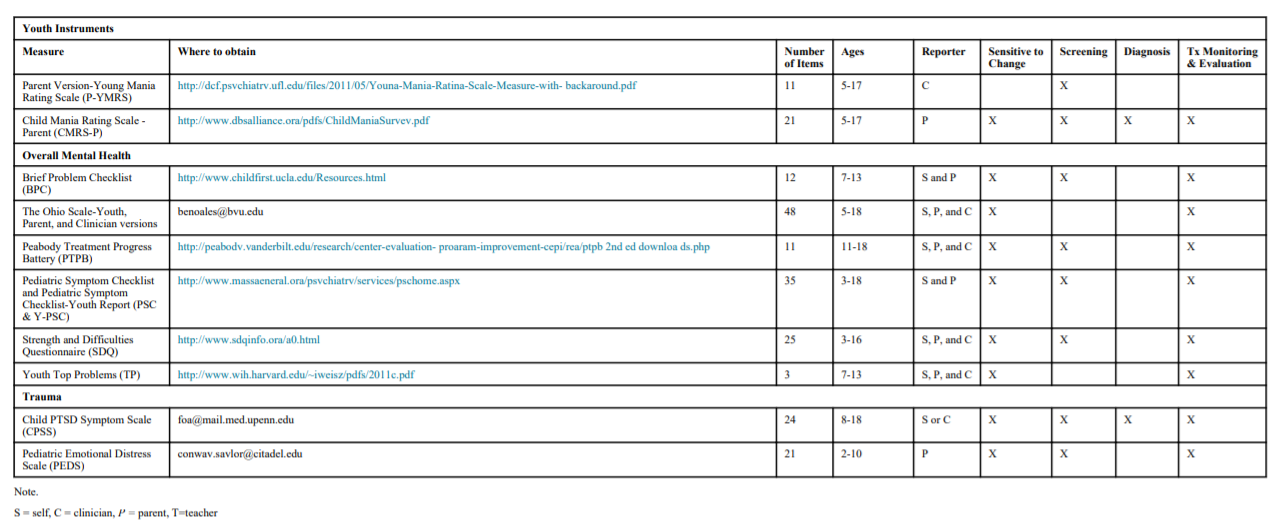
Table 3
Youth Instruments
Youth Instruments Measure Where to obtain Number
of ItemsAges Reporter Sensitive to
ChangeScreening Diagnosis Tx Monitoring
& EvaluationAnxiety Children Yale-Brown Obsessive Compulsive Scale (CY-BOCS) http://icahn.mssm.edu/research/centers/center-of-excellence-for-ocd/rating-scales 10 6-17 P X X X Penn State Worry Questionnaire for Children (PSWQ-C) http://www.childfirst.ucla.edu/Resources.html 16 7-17 S X Revised Children’s Anxiety and Depression Scale Youth and Parent Versions (RCADS/RCADS-P) http://www.childfirst.ucla.edu/Resources.html 47 6-18 S and P X X X X Screen for Child Anxiety Related Emotion Disorders (SCARED) http://psvchiatrv.pitt.edu/sites/default/files/Documents/assessments/SCARED%20Child.pdf 41 6-18 S and P X X X Spence Children’s Anxiety Scale (SCAS) http://www.scaswebsite.com 44 7-19 S and P X X X X Depression Center for Epidemiologic Studies Depression Scale for Children (CES-DC) http://www.bri2htfutures.or2/rnentalhealth/pdf/professionals/bridges/cesdc.pdf 20 6-23 S X X X Depression Self Rating Scale for Children (DSRSC) http://www.scalesandmeasures.net/files/files/Birleson%20Self- Rating%20Scale%20for%20Child%20Depressive%20Disorder.pdf 18 8-14 S X Disruptive Behavior Child and Adolescent Disruptive Behavior Inventory-Parent & Teacher Version (CADBI) http://measures.earlvadolescence.org/measures/view/40/ 25 Not specifi-ed P and T X X Eating Disorder Child Eating Attitudes Test (ChEAT) http://www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/ChEAT.pdf 26 8-13 S X Eating Attitudes Test-26 (EAT-26) http://eat-26.com 26 16-18 S and C X Mania Parent Version-Young Mania Rating Scale (P-YMRS) http://dcf.psvchiatrv.ufl.edu/files/2011/05/Youna-Mania-Ratina-Scale-Measure-with- backaround.pdf 11 5-17 C X Child Mania Rating Scale – Parent (CMRS-P) http://www.dbsalliance.ora/pdfs/ChildManiaSurvev.pdf 21 5-17 P X X X X Overall Mental Health Brief Problem Checklist (BPC) http://www.childfirst.ucla.edu/Resources.html 12 7-13 S and P X X X The Ohio Scale-Youth, Parent, and Clinician versions ude.uvb@selaoneb 48 5-18 S, P, and C X X Peabody Treatment Progress Battery (PTPB) http://peabodv.vanderbilt.edu/research/center-evaluation- proaram-improvement-cepi/rea/ptpb 2nd ed downloa ds.php 11 11-18 S, P, and C X X X Pediatric Symptom Checklist and Pediatric Symptom Checklist-Youth Report (PSC & Y-PSC) http://www.massaeneral.ora/psvchiatrv/services/pschome.aspx 35 3-18 S and P X X X Strength and Difficulties Questionnaire (SDQ) http://www.sdqinfo.ora/a0.html 25 3-16 S, P, and C X X X Youth Top Problems (TP) http://www.wih.harvard.edu/~iweisz/pdfs/2011c.pdf 3 7-13 S, P, and C X X Trauma Child PTSD Symptom Scale (CPSS) ude.nnepu.dem.liam@aof 24 8-18 S or C X X X X Pediatric Emotional Distress Scale (PEDS) ude.ledatic@rolvas.vawnoc 21 2-10 P X X X
I wasn’t able to put the complete Table 3 [HTML] in the above, I recopied the complete Table 3 from the PDF copy. Table 3 below shows the columns which tell you whether a given instrument is useful for Screening, Diagnosis, and/or Therapy Monitoring & Evaluation.
Overall Mental Health
Nine instruments were identified (3 adult, 6 youth) that fell under the category of “overall mental health.”
Adult
Adult instruments ranged in length from 4-41 items. Two adult instruments could be used as screening tools (National Institutes of Health Patient Reported Outcomes Measurement Information System (PROMIS; NIH PROMIS, 2013); Patient Health Questionnaire (PHQ; Spitzer, Kroenke, & Williams, 1999)). The PHQ could also be used as a diagnostic tool. Two instruments could be used for treatment monitoring and evaluation (PHQ, Recovery Assessment Scale (RAS; Giffort, Schmook, Woody, Vollendorf, & Gervain, 1995)).
Youth
Youth instruments ranged from 11-48 items and were intended for administration in youths 3-18. Four of the instruments could be used as screening tools (Brief Problem Checklist (BPC; Chorpita et al., 2010), Peabody Treatment Progress Battery (PTPB; Bickman et al., 2010), Pediatric Symptom Checklist/Youth Report (PSC & Y-PSC; Jellinek et al., 1988), and the Strength and Difficulties Questionnaire (SDQ; Goodman, 1997)). None of the instruments were used as diagnostic tools. All instruments could be used for treatment monitoring and evaluation.
Discussion
As evidenced by this review, there are multiple assessment tools that fit the needs of clinicians in low-resource mental health settings; these measures are free, easily accessible via the Internet or email, brief, have established psychometric properties, and are relevant for the most prevalent mental health disorders. It is our hope that community clinicians will use this compendium to select the most appropriate measure for their general population and specific clients. We have identified 29 adult and 20 youth measures that can be used as part of an EBA toolkit for a heterogeneous group of clients. We also believe that this manuscript can provide a valuable resource for implementation scientists interested in promoting the use of feasible EBA in community settings.
Several exciting national initiatives will make it easier for clinicians to use standardized tools as part of ongoing practice. The National Institutes of Health (NIH) has developed PROMIS, a set of freely available validated measures of patient–reported health status for physical, mental, and social well–being (http://www.nihpromise.org). Although promising, more work must be conducted on the use of these measures in clinical populations (e.g., youth with anxiety and/or depression) given that they have been primarily used in pediatric populations (e.g., oncology). The National Cancer Institute has sponsored a separate, free repository of available standardized tools to assess various mental and physical conditions (https://www.gem-beta.org/). Further, the NIH now requires that articles published from NIH-funded research be freely available to the public, which increases the likelihood of any new measures created through public funding becoming available to practitioners and consumers.