Resource 1 below, Medical Therapy for Heart Failure Caused by Ischemic Heart Disease, has an excellent discussion of heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF).
Here are excerpts focusing mainly on HFrEF from the article (I’ll post excerpts on HFpEF from the article in a seperate post):
Nearly 70% of all HF syndromes can be attributed to underlying IHD.9 . . . . Patients with an obstructive epicardial stenosis (eg, coronary artery disease [CAD]) are more likely to
have HFrEF (rather than HFpEF) as a result of acute ischemic
injury causing MI with scar formation, and large outcomes
trials of treatments with neurohumoral inhibition have clearly
documented reduced adverse outcomes.In contrast, similar treatments in patients with HFpEF have not proven beneficial, and emerging evidence indicates that impaired myocardial perfusion and inflammation, secondary to multiple systemic comorbidities, are key. This therapeutic dilemma may be attributed to the fact that the pathophysiology of HFpEF is heterogeneous, and individuals with this syndrome may have defects in different systemic and myocardial signaling pathways, despite similar clinical presentations and findings.
Management of Patients With CAD and Ischemic Cardiomyopathy (HFrEF)
The development and progression of cardiomyopathy and
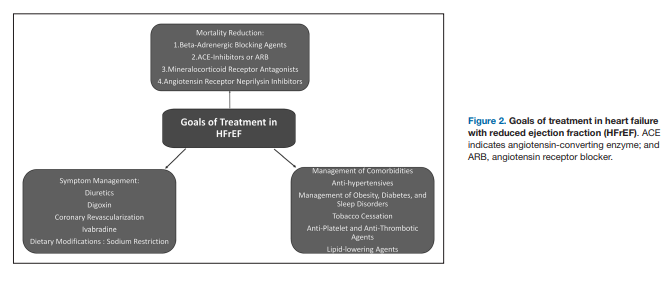
subsequent HFrEF in setting of prior MI or known CAD presents clinicians with multiple management tasks. These areas
require optimized management of comorbid conditions and
pharmacological therapies to improve survival and symptom
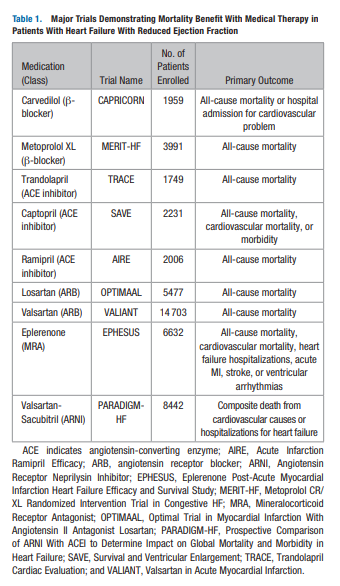
control (Figure 2)Over the past 3 decades, several landmark clinical trials
(Table 1) have provided robust evidence regarding benefit with
the use of pharmacological therapies in patients with HFrEF
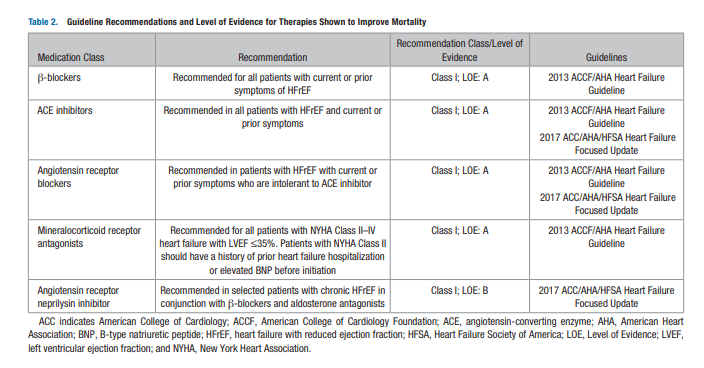
which have been endorsed by the current American College of
Cardiology (ACC)/American Heart Association (AHA)/Heart
Failure Society of America guidelines (Table 2). Notably, this
benefit is observed with long-term adherence to these medical
therapies.Further, there is robust evidence confirming the mortality benefit of primary prevention implantable defibrillators in HFrEF patients with ischemic cardiomyopathy receiving guideline-directed therapy,13,39,40 as well as cardiac resynchronization therapy for select patients with ischemic cardiomyopathy,41 and LV assist devices in patients with refractory HFrEF despite optimal medical and device therapies as a bridge to transplant or destination therapy.42 Most recently, the LV assist device MPC-II trial showed that intramyocardial injection of allogeneic mesenchymal progenitor cells in patients receiving an LV assist device improved temporary weaning in IHD patients with HFrEF. Perhaps more important was the observation of a significantly lower risk of gastrointestinal bleeding,43 offering a potential therapeutic option for these patients in the future.
Medical Therapies for Reducing Adverse Outcomes [in patients with HFrEF]
β-Adrenergic Blocking Agents
β-blocker therapy has been shown to provide survival benefit
in patients with HFrEF secondary to ischemic or nonischemic
cardiomyopathy.44–46 . . . Use of β-blocker therapy for reduction in mortality in patients with remote history of MI or ACS and HFrEF has a Class I, Level of Evidence A recommendation by ACC/AHA and European Society of Cardiology guidelines for HF management.50,51 An important consideration is that the doses of these agents tolerated by HF patients are often limited by lower blood pressures, and only a few reach doses that would produce β-blockade in the true pharmacological sense.ACE Inhibitors and Angiotensin Receptor Blocking Agents
The ACC/AHA and European Society of Cardiology guidelines endorse the use of ACE inhibitors in setting of history of MI or ACS with reduced LVEF, a Class I Level of Evidence A recommendation.50,51
An alternative approach to block the renin-angiotensin system is through AT1 receptor angiotensin receptor blockers
(ARBs). Clearly, these agents work at a final common pathway,
blocking angiotensin II effects. . . . The HF guidelines recommend use of ARB therapy in patients with MI or ACS and subsequent ischemic cardiomyopathy or HFrEF, who are intolerant to ACE inhibitors for reduction in morbidity and mortality.50,51Mineralocorticoid Receptor Antagonists
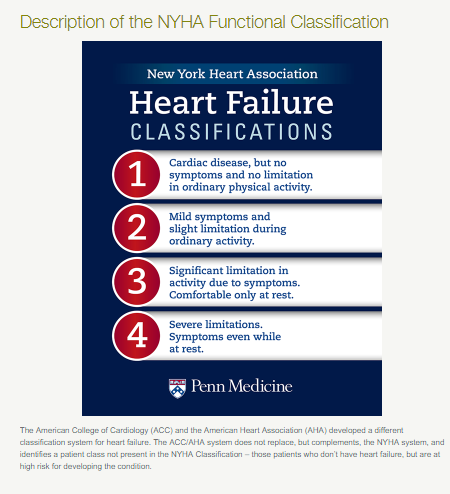
Evidence supports use of mineralocorticoid receptor antagonism in patients with New York Heart Association [Heart Failure Classification] class II–IV HFrEF to reduce morbidity and mortality,58–60 including the subset of patients with ischemic cardiomyopathy.
In patients with HFrEF due to ischemic cardiomyopathy, use of spironolactone has been associated with reversal of negative cardiac remodeling,64 as well as decreased ventricular arrhythmias,65 thereby reducing morbidity risk. Reduction in mortality and morbidity with spironolactone was also seen in a large, randomized placebocontrol trial, where the majority of the patients had HFrEF secondary to ischemic cardiomyopathy.58
The HF guidelines give a Class I, Level of Evidence A recommendation for use of mineralocorticoid receptor antagonists in patients with LVEF ≤35% and New York Heart Association class II–IV HF, unless otherwise contraindicated.50,51
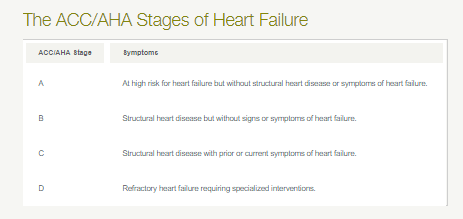
The following three graphics are from Penn Medicine:
Angiotensin Receptor/Neprilysin Inhibitors
Start here.
Resources:
(1) Medical Therapy for Heart Failure Caused by Ischemic Heart Disease [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Circ Res. 2019 May 24;124(11):1520-1535. doi: 10.1161/CIRCRESAHA.118.313568.
(2) A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure With Preserved Ejection Fraction [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Circulation. 2018 Aug 28;138(9):861-870.
The above article has been cited by 6 articles in PubMed Central.
(3) 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Coll Cardiol. 2018 Jan 16;71(2):201-230.
The above article has been cited by 12 articles in PubMed Central.