in this post, I link to and excerpts from PedsCases‘ Management of COVID-19 in Children, by Gauri.Shah Nov 30, 2021.
All that follows is from the above resource:
This podcast discusses the presentation, investigations, and management of COVID-19 in children. It was created by Dr. Gauri Shah, a pediatrician who completed a fellowship in pediatric infectious diseases at the University of Alberta, with close support from Dr. Joan Robinson, a pediatric infectious diseases specialist at the Stollery Children’s Hospital in Edmonton, Canada.
Related Content:
- Podcast: Approach to a Child in Respiratory Distress
- Podcast: Pediatric Chest X-Rays
- Podcast: Acute Management of Croup
- Podcast: Approach to Bronchiolitis
And here are excerpts from the script:
Let’s begin with a case and I will try and highlight the CPS recommendations (2) as we go along managing the case.
Lily Smith is a 6-year-old girl who presented to the emergency with persistent rhinorrhea and dry cough but no fever, vomiting, or diarrhea. She was tachypneic and oxygen
saturation was only 89% on room air. Chest x-ray showed patchy bilateral infiltrates in both lungs. Her mother recently tested positive for COVID-19 and had a viral pneumonia. How should you manage this child with suspected COVID-19?Clinical Presentation
Luckily, for the most part, COVID-19 is a relatively mild infection in children. Most present with mild symptoms and do not need hospital care. Data from CDC suggests hospitalization rates of only 8 per 100,000 children. Children may in fact be more likely to require hospitalization for Multisystem Inflammatory Syndrome in Children or MIS-C which presents with fever and other symptoms and will be described in more detail later.
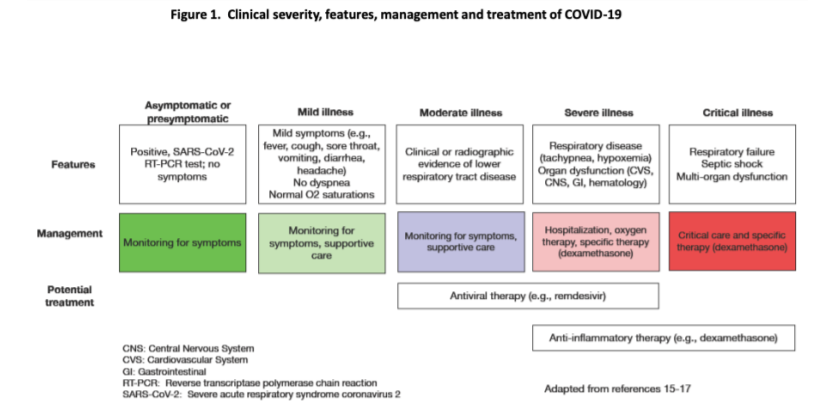
The CPS guidelines discuss the presenting symptoms according to severity of presentation such as
- Asymptomatic ; present with no symptoms but test positive by RT-PCR forSARS-COV2
- Mild illness – Have mild symptoms like fever, sore throat,vomitting, diarrhoes,headaches but no dysneas or desturations
- Moderate illness – shows Clinical and radiologic evidence of lower respiratory tract disease – Monitoring for progression and supportive care is all that is required in above two catogories
- Severe illness – show signs of respiratory disease like tachypnea, hypoximia and may also have s/o organ dysfunction involving the cardivascular, central nervous, GI and hematologic systems . Hospitalization, oxygen and specific therapies are required.
Lily had very few of the long list of possible symptoms but that is the case for mostchildren with COVID-19. Children may be asymptomatic from COVID-19 infection.
Children with pre-existing medical conditions may be at higher risk for severe disease. Some of the conditions which may be perceived as high risk include
● conditions like congenital heart disease, chronic lung disease, sickle cell disease,
● Obesity, diabetes, moderate to severe asthma
● Disorders of coagulation – which may have higher risk of thrombosis.However, most children do not require hospitalization even if they have multiple underlying conditions.
Infection Prevention and Control
Times have changed so much in this last year! Now every potential patient encounter is fraught with risk of inadvertent spread of COVID-19 within the facility and hence strict attention to all the recommended precautions to prevent and limit the spread of the disease become crucial.
You strongly suspect COVID-19 for Lily given the presentation and you have examined her safely. You step out of the room (and doff safely and wash your hands between all steps!) and plan your diagnostic strategy.
COVID-19 is diagnosed with Polymerase Chain Reactino (PCR) testing. There are two indications for diagnostic testing: first when you suspect COVD-19 infection in the symptomatic patient like Lily and the other for asymptomatic testing of close contacts of a case.
The most common samples collected are nasopharyngeal (NP) swabs. Other potentialvsamples include the throat and saliva swabs. NP swabs are preferred due to higher specificity of 99.2% and sensitivity of 83.2% in the diagnosis of COVID19.
START HERE