The single best resource on the evaluation of liver blood test abnormalities is the article referenced and excerpted in my post, Excerpts From The 2017 Guidelines On The Evaluation Of Abnormal Liver Tests From The ACG, posted on April 26, 2019 by Tom Wade MD.
Basically, though, the above American guideline like the British guideline of this post are the same. Order a bunch of liver tests and then consider referring the patient to a GI doctor or even better, to a liverspecialist .*
*Here is recommendation 10 from the British Society of Gastroenterology:
- Recommendation 10: Adults with abnormal liver blood
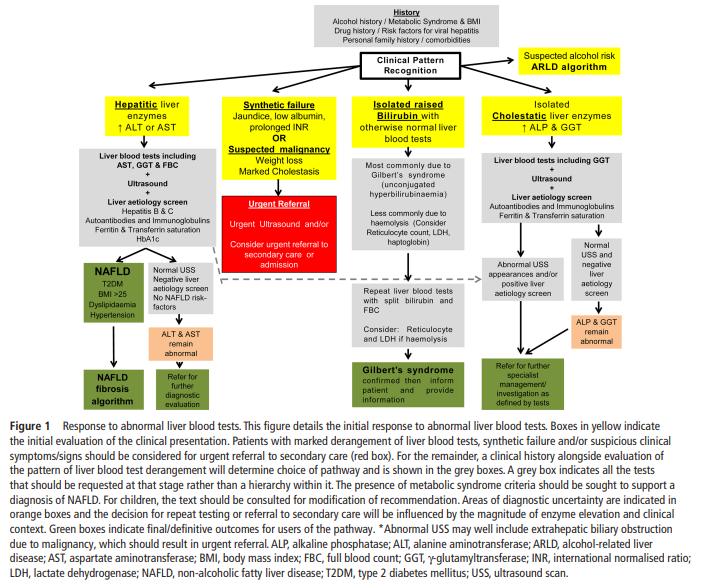
tests, even with a negative extended liver aetiology screen and no risk factors for NAFLD, should be referred/discussed to a gastroenterologist with an interest in liver disease/hepatologist for further evaluation (figure 1). (level 4, grade C)
This post contains links to and excerpts from Resource (1) below, 2018 Guidelines on the management of abnormal liver blood tests [PubMed Abstract], from the British Society of Gastroenterology.
Here are the excerpts:
Recommendations list
- Recommendation 1: Initial investigation for
potential liver disease should include bilirubin,
albumin, alanine aminotransferase (ALT), alkaline phosphatase (ALP) and γ-glutamyltransferase (GGT), together with a full blood count
if not already performed within the previous 12
months. (level 2b, grade B)
► Research Recommendation 1: Further evidence
is required to establish the cost-effectiveness
of case finding for non-alcoholic fatty liver
disease (NAFLD) in high-risk groups before it
can be recommended. (level 5, grade D)Recommendation- 2: Abnormal liver bloodtest results should only be interpreted after review of the previous results, past medicalhistory and current medical condition. (level 5,
grade D)- Recommendation 3: The extent of liver blood
test abnormality is not necessarily a guide to
clinical significance. This is determined by the
specific analyte which is abnormal (outside the
reference range) and the clinical context. (level
5, grade D)- Recommendation 4: Patients with abnormal
liver blood tests should be considered for
investigation with a liver aetiology screen irrespective of level and duration of abnormality.
Abnormal refers to an analyte which is outside
the laboratory reference range (level 2b,
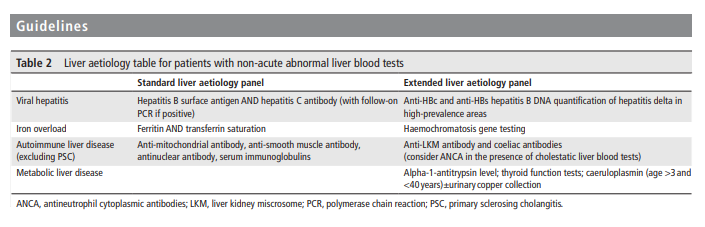
grade B)- Recommendation 5: In adults a standard liver
aetiology screen should include abdominal
ultrasound scan (USS), hepatitis B surface
antigen, hepatitis C antibody (with follow-on
polymerase chain reaction (PCR) if positive),
anti-mitochondrial antibody, anti-smooth
muscle antibody, antinuclear antibody, serum
immunoglobulins, simultaneous serum
ferritin and transferrin saturation. (level 2b,
grade C)- Recommendation 6: In children, ferritin and
transferrin saturation may not be indicated,
but autoantibody panel should include antiliver kidney microsomal antibody and coeliac
antibodies. Alpha-1-antitrypsin level and caeruloplasmin (age >3 years) should be included,
and abnormalities discussed with an appropriate inherited metabolic disease specialist.
(level 2b, grade C)- Recommendation 7: Adults with NAFLD
should undergo risk stratification to determine
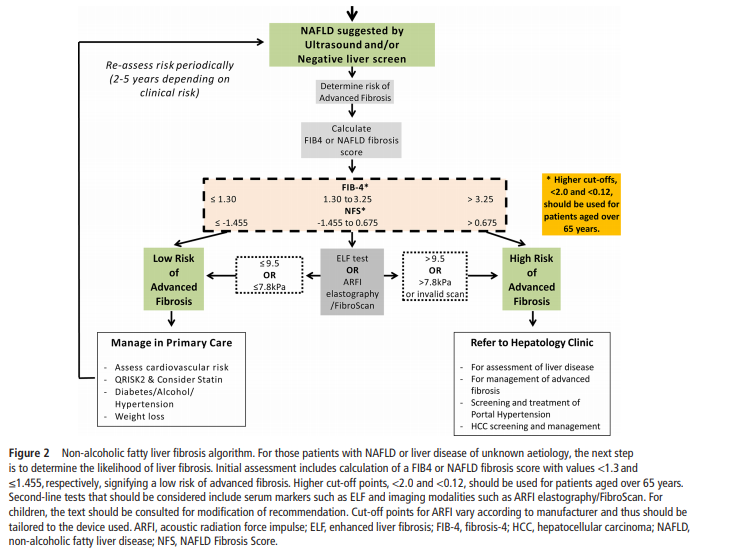
the extent of their liver fibrosis (figures 1 and 2).
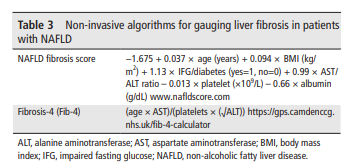
– First-line testing should use either fibrosis-4
(FIB-4) or NAFLD Fibrosis Score (NFS)
– see table 3 (level 2b, grade B). Calculation facilities for FIB-4 and NFS should be incorporated in all primary care computer systems. (level 5, grade D)
– Second-line testing requires a quantitative assessment of fibrosis with tests such as serum enhanced liver fibrosis (ELF) measurements or Fibroscan/acoustic radiation force
impulse (ARFI) elastography. (level 2b, grade B)
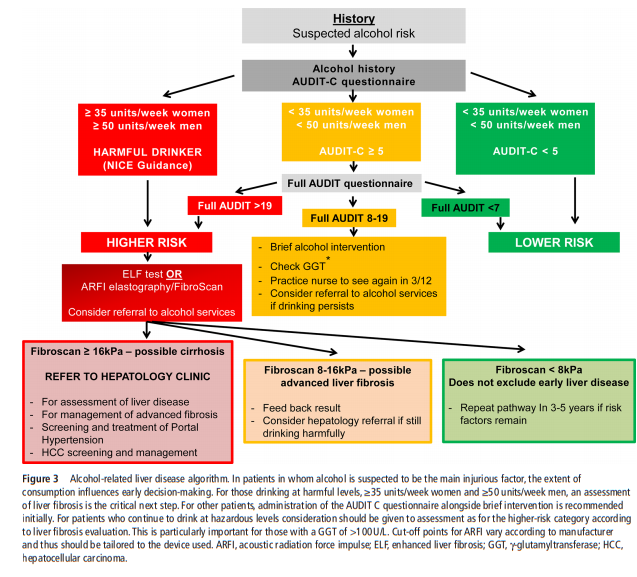
– We recommend that hepatologists at a local level champion this idea and discuss it with commissioners of health to deal with the burden of liver disease in their area- Recommendation 8: Consider referral to alcohol services for all adults with alcohol-related liver disease (ARLD) with evidence of alcohol dependency as defined by an AUDIT score of >19. (level 3b, grade C)
- Recommendation 9: Harmful drinkers should undergo risk stratification with clinical assessment and Fibroscan/ARFI elastography. Adults should be referred to secondary care if there is evidence of advanced liver disease (features of cirrhosis or portal hypertension on imaging or from blood tests) and/or Fibroscan reading is >16kPa (if available).
(level 2b, grade B)- Research Recommendation 2: Further evidence is required to establish the most cost-effective approach to identify patients with ARLD and NAFLD at risk of having advanced liver fibrosis.
- Recommendation 10: Adults with abnormal liver blood
tests, even with a negative extended liver aetiology screen and no risk factors for NAFLD, should be referred/discussed to a gastroenterologist with an interest in liver disease/hepatologist for further evaluation (figure 1). (level 4, grade C)
Text
Text
Text
Text
Resources
(1) Guidelines on the management of abnormal liver blood tests [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Gut. 2018 Jan;67(1):6-19. doi: 10.1136/gutjnl-2017-314924. Epub 2017 Nov 9.
(2) ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries [PubMed Abstract] [Full Text PDF] Am J Gastroenterol. 2017 Jan;112(1):18-35. doi: 10.1038/ajg.2016.517. Epub 2016 Dec 20.