ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries is an outstanding resource for all clinicians [PubMed Abstract] [Full-Text HTML] [Download the PDF from the HTML] Am J Gastroenterol. 2017 Jan;112(1):18-35. doi: 10.1038/ajg.2016.517. Epub 2016 Dec 20.
This post contains excerpts from the above article:
Abstract:
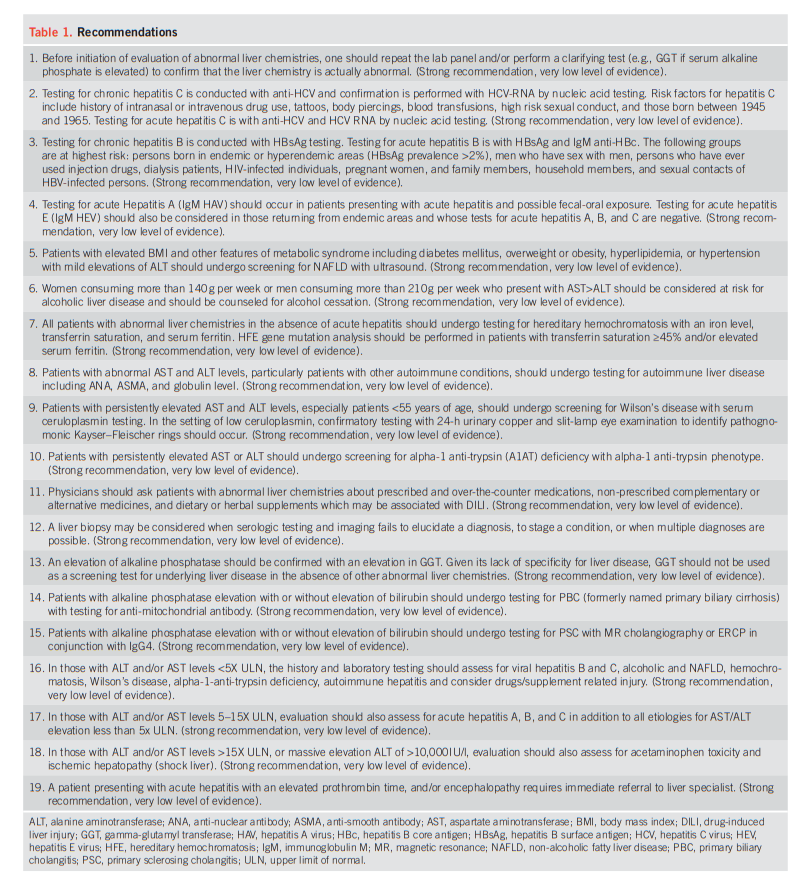
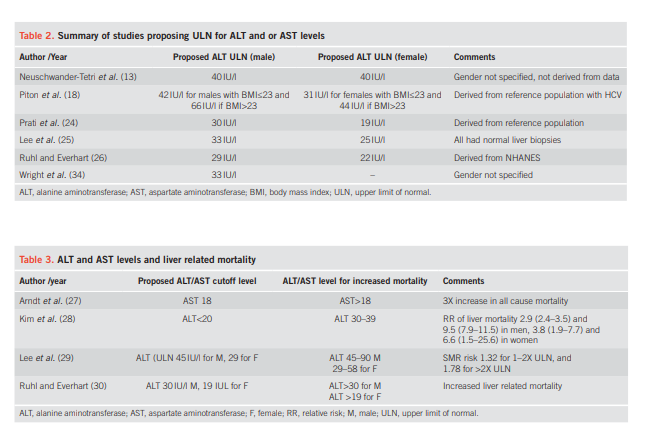
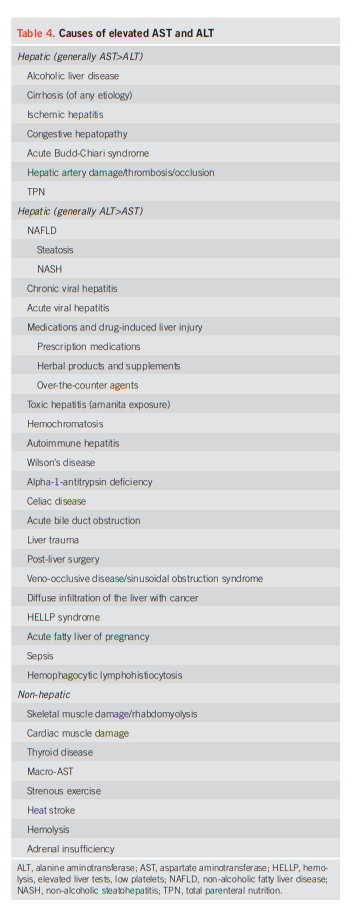
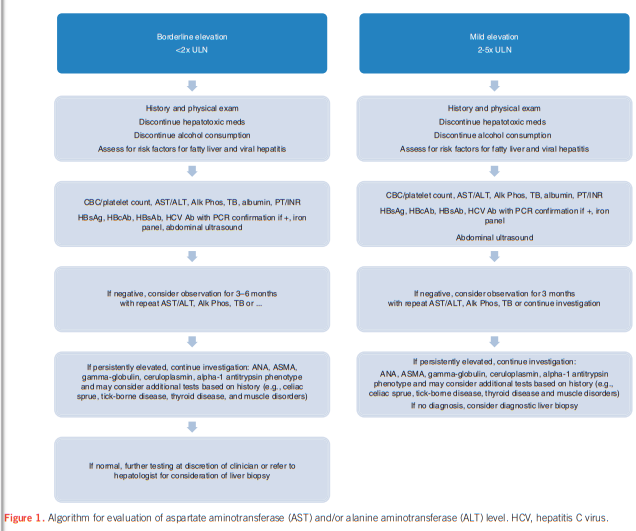
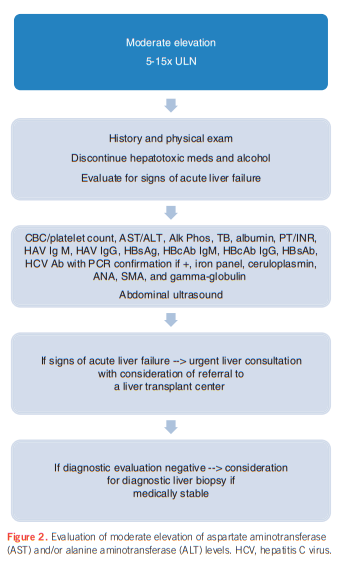
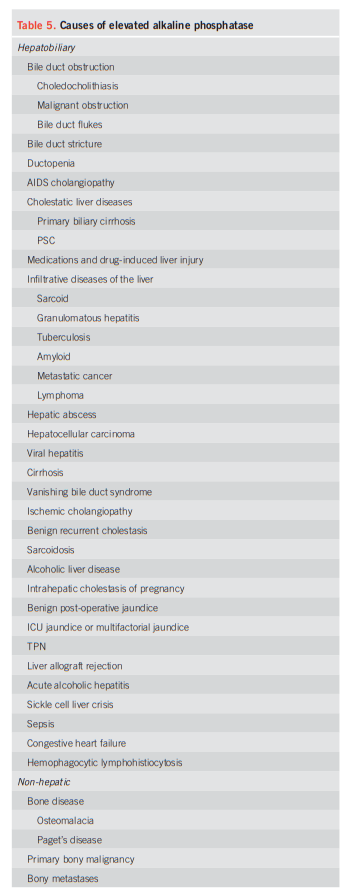
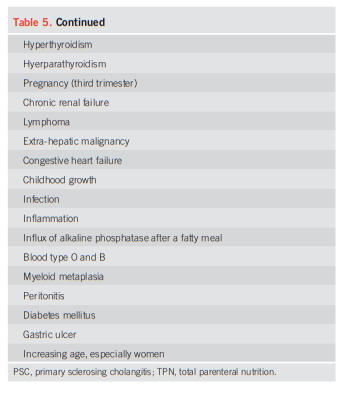
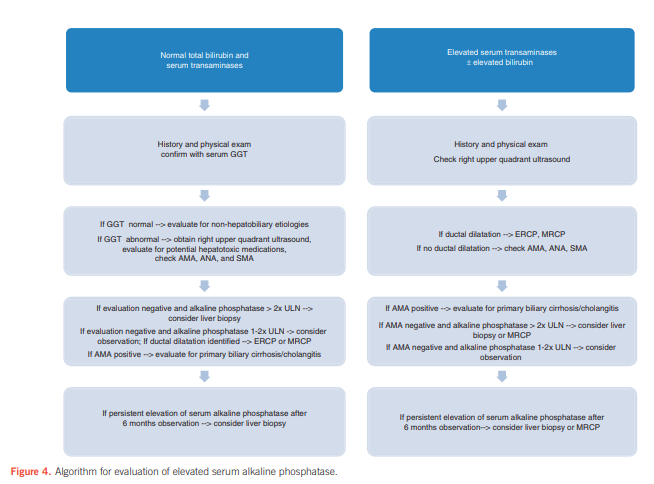
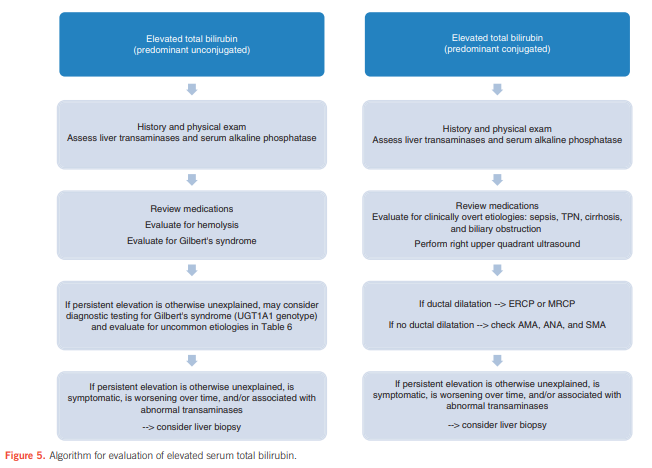
Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defined as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defined as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. The evaluation of hepatocellular injury includes testing for viral hepatitis A, B, and C, assessment for nonalcoholic fatty liver disease and alcoholic liver disease, screening for hereditary hemochromatosis, autoimmune hepatitis, Wilson’s disease, and alpha-1 antitrypsin deficiency. In addition, a history of prescribed and over-the-counter medicines should be sought. For the evaluation of an alkaline phosphatase elevation determined to be of hepatic origin, testing for primary biliary cholangitis and primary sclerosing cholangitis should be undertaken. Total bilirubin elevation can occur in either cholestatic or hepatocellular diseases. Elevated total serum bilirubin levels should be fractionated to direct and indirect bilirubin fractions and an elevated serum conjugated bilirubin implies hepatocellular disease or biliary obstruction in most settings. A liver biopsy may be considered when serologic testing and imaging fails to elucidate a diagnosis, to stage a condition, or when multiple diagnoses are possible.
These recommendations are intended for use by physicians and health care providers and suggest preferred approaches to the diagnoses and evaluation of those with abnormal liver tests.
Resources:
(1) ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries is an outstanding resource for all clinicians [PubMed Abstract] [Full Text PDF] Am J Gastroenterol. 2017 Jan;112(1):18-35. doi: 10.1038/ajg.2016.517. Epub 2016 Dec 20.
(2) EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis [PubMed Citation] [Full Text HTML] [Full Text PDF]. J Hepatol. 2015 Jul;63(1):237-64. doi: 10.1016/j.jhep.2015.04.006. Epub 2015 Apr 21.
(3) Clinical Practice Guidelines [This link is to 25 Guidelines on Liver Diseases] from the Journal of Hepatology of The European Society for the Study of the Liver (EASL)