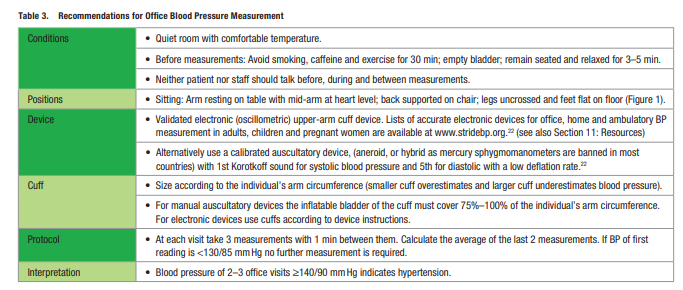
In this post I link to and excerpt from the 2020 International Society of Hypertension Global Hypertension Practice Guidelines [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Hypertension. 2020 Jun;75(6):1334-1357.
I reviewed and excerpted from the great Curbsiders’ post and podcast on hypertension [Direct link to their post and podcast] in Links To And Excerpts From The Curbsiders’ #254 Hypertension Update With Additional Resources On Primary Aldosteronism. Posted on February 5, 2021 by Tom Wade MD
And see also Everyone Needs An Accurate Home Blood Pressure Machine – Here Are Two Websites With Lists Of Accurate BP Machines To Purchase. Posted on February 6, 2021 by Tom Wade MD
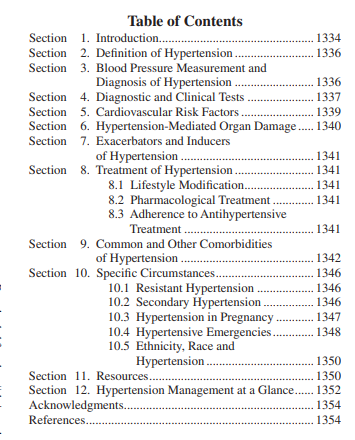
Here are excerpts from the 2020 ISH Global Hypertension Guidelines:
Section 1: Introduction
Context and Purpose of This Guideline
Raised BP remains the leading cause of death globally,
accounting for 10.4 million deaths per year.3 When reviewing global figures, an estimated 1.39 billion people had hypertension in 2010. 4 However, BP trends show a clear shift of the highest BPs from high-income to low-income regions,5 with an estimated 349 million with hypertension in HIC and 1.04 billion in LMICs.4Recently, we have observed a recent flurry of updated evidence-based guidelines arising mainly from high-income regions and countries, including the United States of America,2 Europe,1 United Kingdom,8 Canada9 and Japan.10
New developments include redefining hypertension,2 initiating treatment with a single pill combination therapy,1 advising wider out-of-office BP measurement,2,10 and lower BP targets.1,2,8,11,12
Section 2: Definition of Hypertension
Section 3: Blood Pressure Measurement and
Diagnosis of HypertensionEssential
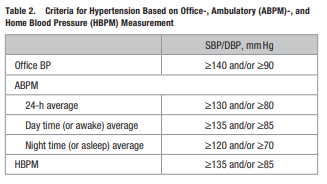
Hypertension Diagnosis – Office BP Measurement
• The measurement of BP in the office or clinic is most commonly the basis for hypertension diagnosis and follow-up. Office BP should be measured according to recommendations shown in Table 3 and Figure 1.1,2,17,18
• Whenever possible, the diagnosis should not be made
on a single office visit. Usually 2–3 office visits at
1–4-week intervals (depending on the BP level) are
required to confirm the diagnosis of hypertension.
The diagnosis might be made on a single visit, if BP is ≥180/110 mmHg and there is evidence of cardiovascular disease (CVD).1,2,17,18
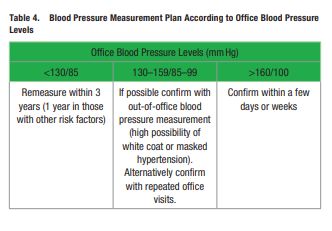
• The recommended patient management according to
office BP levels is presented in Table 4.
• If possible and available, the diagnosis of hypertension should be confirmed by out-of-office BP measurement (see below).1,2,19–21Optimal
Hypertension Diagnosis – Office Blood Pressure
Measurement
• Initial evaluation: Measure BP in both arms, preferably simultaneously. If there is a consistent difference
between arms >10 mmHg in repeated measurements, use the arm with the higher BP. If the difference is >20 mmHg consider further investigation.
• Standing blood pressure: Measure in treated hypertensives after 1 min and again after 3 min when there
are symptoms suggesting postural hypotension and at
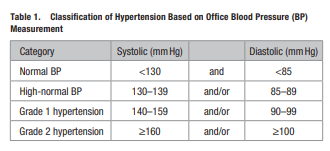
the first visit in the elderly and people with diabetes. • Unattended office blood pressure: Multiple automated BP measurements taken while the patient remains alone in the office provide a more standardized evaluation but also lower BP levels than usual office measurements with uncertain threshold for hypertension diagnosis.17,18,23,24 Confirmation with out of-office BP is again needed for most treatment decisions.Hypertension Diagnosis – Out-of-Office Blood
Pressure Measurement• Out-of-office BP measurements (by patients at home
or with 24-hour ambulatory blood pressure monitoring [ABPM]) are more reproducible than office
measurements, more closely associated with hypertension-induced organ damage and the risk of cardiovascular events and identify the white coat and
masked hypertension phenomena (see below).
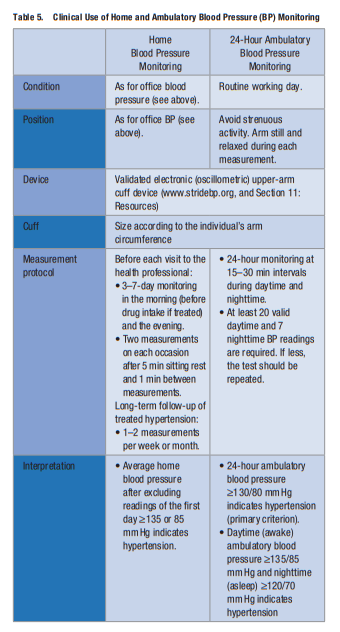
• Out-of-office BP measurement is often necessary for
the accurate diagnosis of hypertension and for treatment decisions. In untreated or treated subjects with
office BP classified as high-normal BP or grade 1 hypertension (systolic 130–159 mmHg and/or diastolic
85–99 mmHg), the BP level needs to be confirmed using home or ambulatory BP monitoring (Table 5).1,2,17,21
• Recommendations for performing home and ambulatory BP measurement are presented in Table 5.
White Coat and Masked Hypertension
• The use of office and out-of-office (home or ambulatory)
BP measurements identifies individuals with white coat
hypertension, who have elevated BP only in the office
(nonelevated ambulatory or home BP), and those with
masked hypertension, who have nonelevated BP in the
office but elevated BP out of the office (ambulatory or
home).1,2,17–21,25–27 These conditions are common among
both untreated subjects and those treated for hypertension. About 10%–30% of subjects attending clinics due
to high BP have white coat hypertension and 10%–15%
have masked hypertension.
• White coat hypertension: These subjects are at intermediate cardiovascular risk between normotensives and
sustained hypertensives. The diagnosis needs confirmation with repeated office and out-of-office BP measurements. If their total cardiovascular risk is low and there is no hypertension-mediated organ damage (HMOD), drug treatment may not be prescribed. However, they should be followed with lifestyle modification, as they may develop sustained hypertension requiring drug treatment.1,2,17–21,25–27
• Masked hypertension: These patients are at similar risk
of cardiovascular events as sustained hypertensives. The
diagnosis needs confirmation with repeated office and
out-of-office measurements. Masked hypertension may
require drug treatment aiming to normalize out-of-office
BP.1,2,17–21,25–27Section 4: Diagnostic /Clinical Tests
See pp 1338 + 1339 for details.
Section 5: Cardiovascular Risk Factors
Diagnostic Approach
• More than 50% of hypertensive patients have additional
cardiovascular risk factors.28,29
• The most common additional risk factors are diabetes
(15%–20%), lipid disorders (elevated low-density lipoprotein-cholesterol [LDL-C] and triglycerides [30%]), overweight-obesity (40%), hyperuricemia (25%) and metabolic
syndrome (40%), as well as unhealthy lifestyle habits (eg,
smoking, high alcohol intake, sedentary lifestyle).28–30
• The presence of one or more additional cardiovascular
risk factors proportionally increases the risk of coronary, cerebrovascular, and renal diseases in hypertensive • The therapeutic strategy must include lifestyle changes,
BP control to target and the effective treatment of the
other risk factors to reduce the residual cardiovascular
risk.
• The combined treatment of hypertension and additional
cardiovascular risk factors reduces the rate of CVD beyond BP control.Other Additional Risk Factors
• Elevated serum uric acid (s-UA) is common in patients
with hypertension and should be treated with diet, urate
influencing drugs (losartan, fibrates, atorvastatin) or urate lowering drugs in symptomatic patients (gout with
s-UA >6mg/dl [0.357 mmol/L]).
• An increase in cardiovascular risk must be considered
in patients with hypertension and chronic inflammatory diseases, chronic obstructive pulmonary disease
(COPD), psychiatric disorders, psychosocial stressors
where an effective BP control is warranted.Essential
• An evaluation of additional risk factors should be
part of the diagnostic workup in hypertensive patients particularly in the presence of a family history
of CVD.
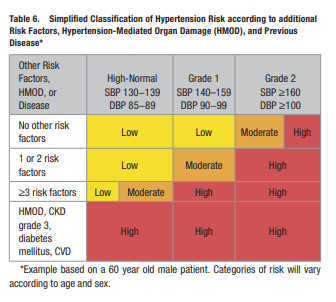
• Cardiovascular risk should be assessed in all hypertensive patients by easy-to-use scores based on
BP levels and additional risk factors according to a
simplified version of the approach proposed by ESCESH Guidelines (Table 6).1
• A reliable estimate of cardiovascular risk can be obtained in daily practice by including:
• Other Risk Factors: Age (>65 years), sex
(male>female), heart rate (>80 beats/min), increased
body weight, diabetes, high LDL-C/triglyceride, family history of CVD, family history of hypertension,
early-onset menopause, smoking habits, psychosocial
or socioeconomic factors. HMOD: LVH (LVH with
ECG), moderate-severe CKD (CKD; eGFR <60 ml/
min/1.73m2), any other available measure of organ
damage. Disease: previous coronary heart disease
(CHD), HF, stroke, peripheral vascular disease, atrial
fibrillation, CKD stage 3+.
Section 6: Hypertension-Mediated Organ
Damage (HMOD)Definition and Role of HMOD in Hypertension
ManagementHypertension-mediated organ damage (HMOD) is defined as
the structural or functional alteration of the arterial vasculature and/or the organs it supplies that is caused by elevated BP.
End organs include the brain, the heart, the kidneys, central
and peripheral arteries, and the eyes.While assessment of overall cardiovascular risk is important for the management of hypertension, additional detection of HMOD is unlikely to change the management of those patients already identified as high risk (ie, those with established CVD, stroke, diabetes, CKD, or familial hypercholesterolemia). However, it can provide important therapeutic guidance on (1) management for hypertensive patients with low or moderate overall risk through reclassification due to presence of HMOD, and (2) preferential selection of drug treatment based on the specific impact on HMOD.1
Section 7: Exacerbators and Inducers of
HypertensionBackground
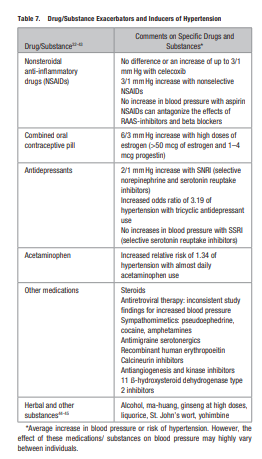
Several medications and substances may increase BP or antagonize the BP-lowering effects of antihypertensive therapy
in individuals (Table 7). It is important to note that the individual effect of these substances on BP can be highly variable with greater increases noted in the elderly, those with
higher baseline BP, using antihypertensive therapy or with
kidney disease.
Section 8: Treatment of Hypertension
Start here.